Colorectal cancer was the second most common cancer in Ireland. It accounted for 13% of all malignant neoplasms, excluding non-melanoma skin cancer, in women and 15% in men (Table 5.1). The annual average number of new cases diagnosed was 1,307 in women and 1,631 in men. 63% of these cancers arose in the colon and 37% in the rectum. During 1995-2007, the number of new cases increased, on average, by approximately 2% per annum, but during 2002-2007 increased by 4% per annum. The patterns of increase were similar for RoI and NI.
The risk of developing colorectal cancer up to the age of 74 was 1 in 32 for women and 1 in 20 for men and was similar for NI and RoI. At the end of 2008, 2,335 women and 2,787 men aged under 65, and 6,137 women and 7,205 men aged 65 and over, were alive up to 15 years after their colorectal cancer diagnosis.
Table 5.1 Summary information for colorectal cancer in Ireland, 1995-2007
Ireland | RoI | NI | ||||
female | male | female | male | female | male | |
% of all new cancer cases | 9% | 11% | 9% | 10% | 10% | 11% |
% of all new cancer cases excluding non-melanoma skin cancer | 13% | 15% | 12% | 15% | 13% | 15% |
average number of new cases per year | 1307 | 1631 | 849 | 1114 | 458 | 517 |
cumulative risk to age 74 | 3.2% | 5.1% | 3.1% | 5.1% | 3.2% | 5.0% |
15-year prevalence (1994-2008) | 8472 | 9992 | 5487 | 6789 | 2985 | 3203 |
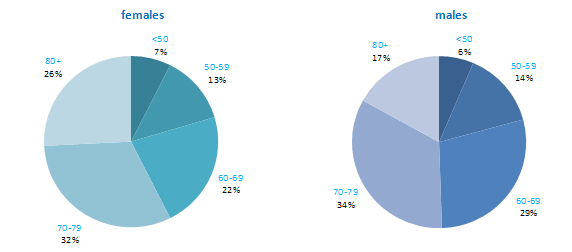
Approximately half of colorectal cancers were diagnosed in those aged 70 and older—51% of men and 58% of women (Figure 5.1). The age distribution was similar for both sexes, although there was a higher proportion of cases in men aged 60–69 (29%, compared to 22% in women) and a higher proportion in women aged 80 and older (26%, compared to 17% in men).
Figure 5.1 Age distribution of colorectal cancer cases in Ireland, 1995-2007, by sex
The incidence of colorectal cancer among both men and women in RoI and NI was close to the median for the countries shown. Rates were highest in New Zealand among women and in the Czech Republic for men (Figure 5.2).
Figure 5.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: colorectal cancer | |
| females | males |
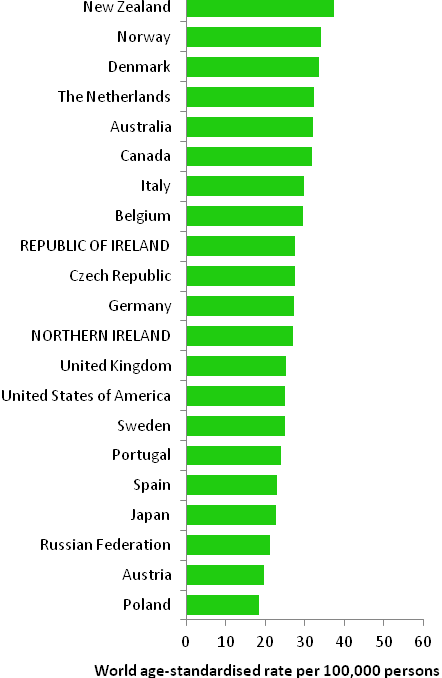 | 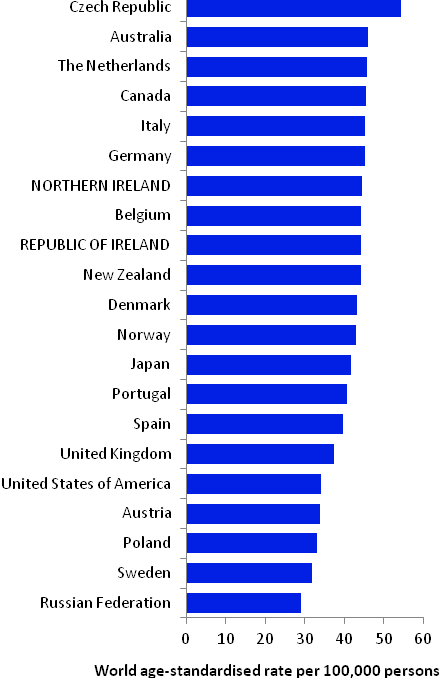 |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from cancer registry data for 2005-2007) | |
Table 5.2 Risk factors for colorectal cancer, by direction of association and strength of evidence
Increases risk | Decreases risk | |
Convincing or probable | Family history of colorectal cancer1,2 | Physical activity5,6,13 |
| Tobacco smoking3,4 | Hormone replacement therapy14 |
| Alcohol4 | Oral contraceptives14,15 |
| Greater body fatness, in particular, abdominal fatness5,6 | Aspirin and other non-steroidal anti-inflammatory drugs16 |
| Red and processed meat6 | Foods containing dietary fibre6 |
| Asbestos7 | Garlic6 |
| Ionizing radiation3,8 | |
Possible | Disinfection by-products in drinking water9 | Non starchy vegetables6,17 |
Helicobacter pylori infection10 | Fruit6,17 | |
Insulin-like growth factor-1 (IGF-1)11 | Folate18 | |
Diabetes12 | Fish6 | |
Coffee19 | ||
Vitamin B620,21 | ||
Soya22,23 | ||
Milk, dairy and/or calcium24 | ||
Vitamin D25,26 | ||
| ||
1 First degree relative(s) with colorectal cancer; 2 Johns and Houlston, 2001; 3 colon cancer only; 4 Secretan et al., 2009; 5 International Agency for Research on Cancer, 2002; 6 World Cancer Research Fund / American Institute for Cancer Research, 2007; 7 Straif et al., 2009; 8 El Ghissassi et al., 2009; 9 Rahman et al., 2010; 10 Zhao et al., 2008; 11 Rinaldi et al., 2010; 12 Larsson et al., 2005; 13 Harriss et al., 2009; 14 International Agency for Research on Cancer, 2011a; 15 Bosetti et al., 2009; 16 International Agency for Research on Cancer, 1997; 17 International Agency for Research on Cancer, 2003; 18 Kennedy et al., 2011; 19 Galeone et al., 2010; 20 intake and blood levels; 21 Larsson et al., 2010; 22 in women only; 23 Yan et al., 2010; 24 Huncharek et al., 2009; 25 blood levels; 26 Yin et al., 2009 | ||
Up to 10% of colorectal cancers are hereditary and most are due to the genetic syndromes of familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (HNPCC) (Hawkins and Ward, 2001). Excluding these syndromes, individuals who have a first degree relative with colorectal cancer have around a two-fold increased risk of developing the disease themselves.
Lifestyle factors are extremely important in colorectal cancer (Table 5.2). Smoking is causally related to colon, but not rectal, cancer. Alcohol is a cause of both colon and rectal cancers. Higher levels of body fatness, and in particular central adiposity, are positively related to risk. In a recent meta-analysis, each 5kg/m2 increment in body mass index was associated with an 18% increase in risk; the association appears stronger for colon than rectal cancer, for men than women, and in studies adjusting for physical activity (Ning et al., 2010). In contrast, physical activity is consistently inversely associated with colon cancer, in particular, and risk decreases in a dose-response fashion with increased frequency or intensity of activity. Regular use of aspirin or other non-steroidal anti-inflammatory drugs may reduce colorectal cancer risk by up to half. In addition, risk is decreased in women taking hormone replacement therapy and is likely also to be lower in those who have taken oral contraceptives.
Many studies have found increased risk in individuals who have higher intakes of processed meats (preserved by smoking, curing or salting, such as ham, bacon or salami) and red meats. In contrast, higher intake of various other dietary components may be associated with lower risk, including garlic; fruit; fish; non-starchy vegetables; milk, dairy products or calcium; coffee; soya and soya foods; and foods containing dietary fibre or the B vitamin folate.
Figure 5.3 Adjusted relative risks (with 95% confidence intervals) of colorectal cancer by socio-economic characteristics of geographic area of residence: males
| MalesAmong men there was no significant difference in risk of colorectal cancer between RoI and NI when adjusted for age alone. However, after adjustment for age and socio-economic factors colorectal cancer risk was lower in NI than in RoI (RR=0.92, 95%CI=0.89-0.96) (Figure 5.3). Male colorectal cancer was positively associated with population density, with men resident in the most densely populated areas 14% more likely to develop colorectal cancer than those in the least densely populated areas. Similarly, unemployment was associated with male colorectal cancer, with a steady increase in risk as unemployment in an area increased. Colorectal cancer risk was not related to area-based educational attainment. Persons resident in areas with the highest proportion of persons aged 75 and over living alone had a 10% greater risk of colorectal cancer than those resident in areas with the lowest proportion. |
Figure 5.4 Adjusted relative risks (with 95% confidence intervals) of colorectal cancer by socio-economic characteristics of geographic area of residence: females
| FemalesThere was no significant difference between RoI and NI in the risk of colorectal cancer for women when adjusted for age, or when adjusted for age and socio-economic factors (Figure 5.4). While female colorectal cancer risk was associated with population density, the association was weaker than for men, with the relative risk 4% greater in the most, compared to the least, densely populated areas. Neither unemployment nor educational attainment was associated with female colorectal cancer risk. Areas with higher proportions of persons aged 75 and over living alone had a greater risk of female colorectal cancer. This relationship was slightly stronger for women than men. |
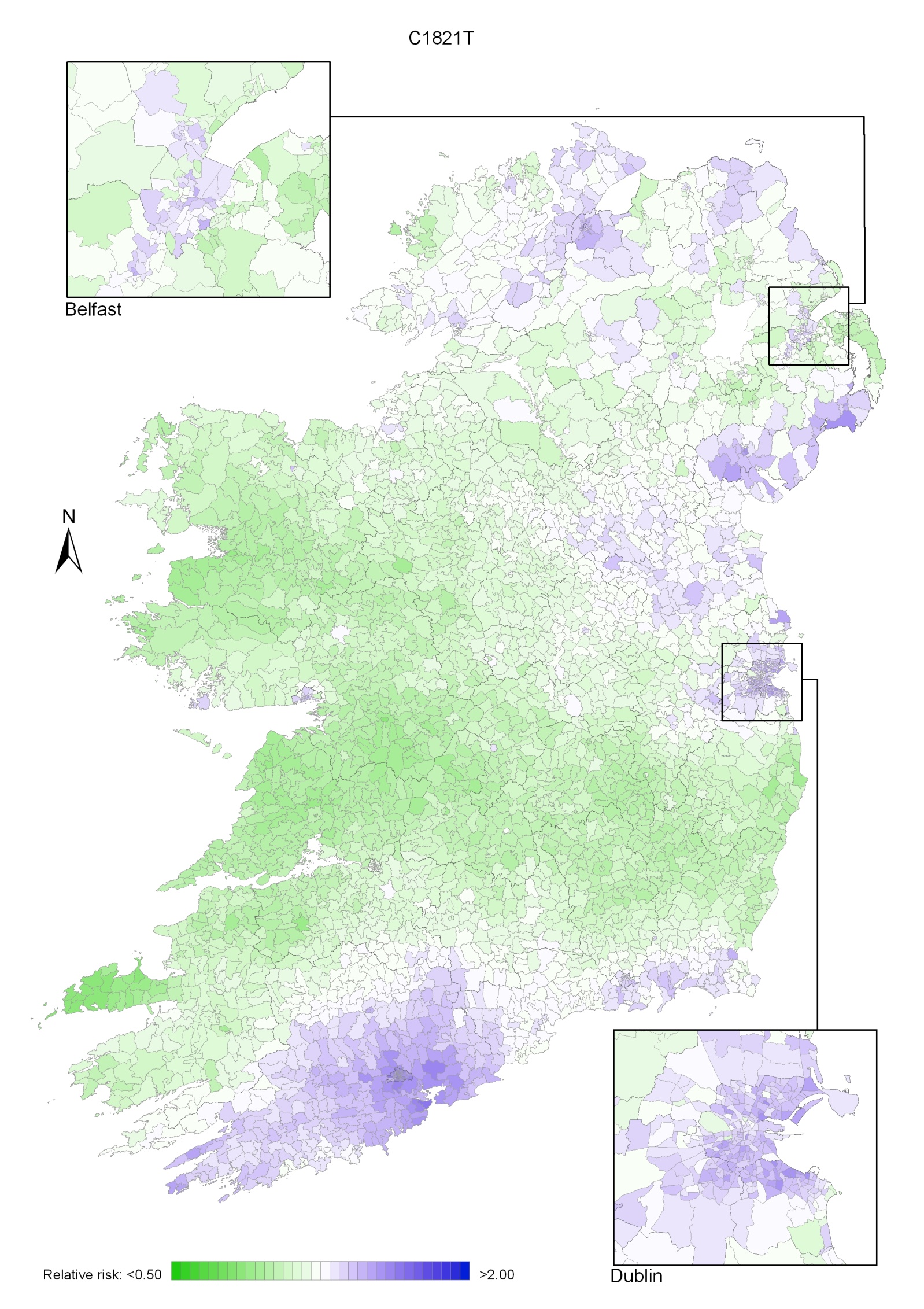
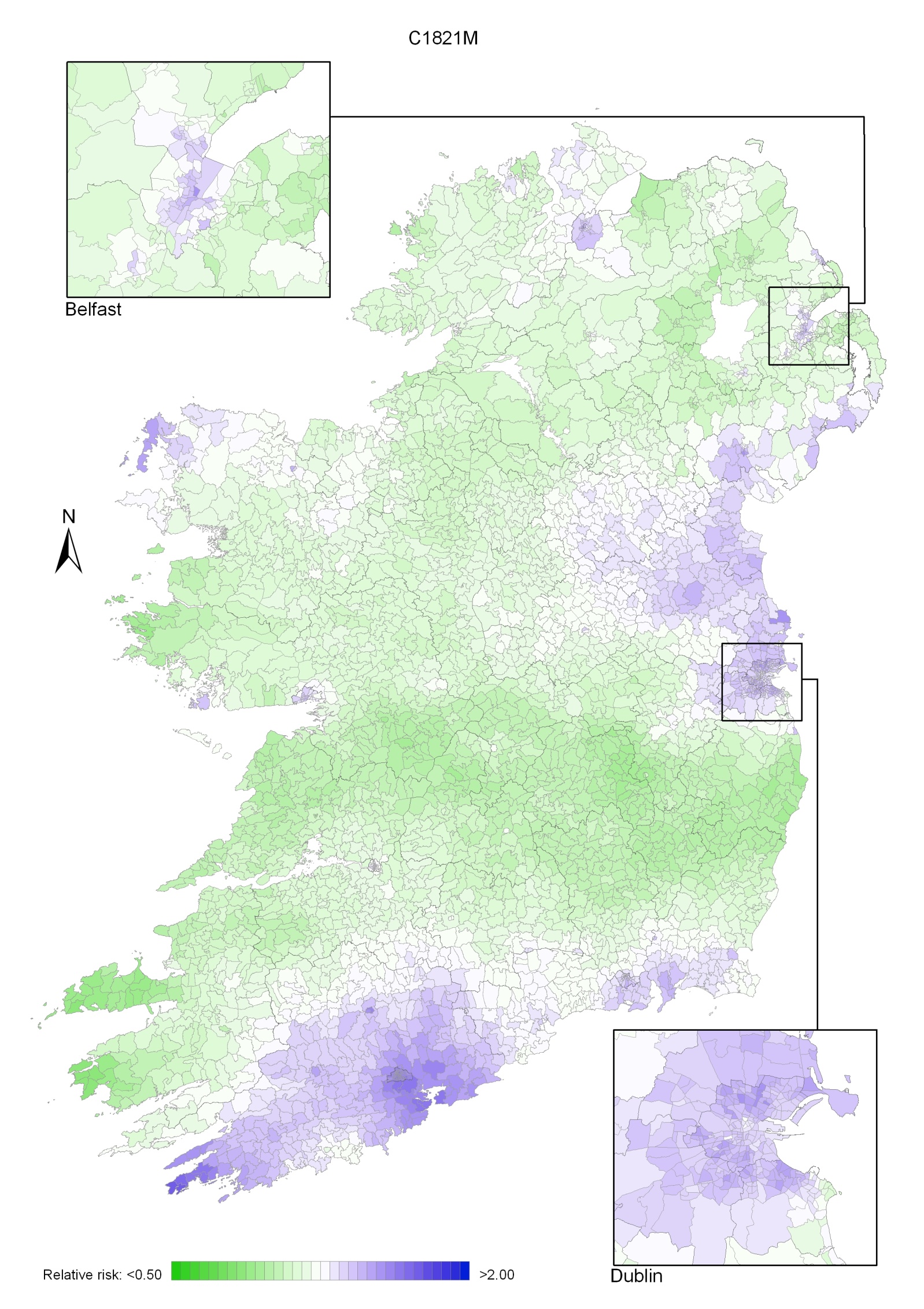
Although the geographical variation in relative risk was fairly modest, there were distinct areas of higher relative risk for colorectal cancer for both men and women (Maps 5.1-5.3).
The pattern for both sexes combined showed a higher relative risk around Cork city and county, with a diffuse pattern in the north extending in a band from Donegal across to Dublin and to a lesser extent in south Waterford and Wexford (Map 5.1).
The pattern for men also showed higher relative risk around Cork and extending south-west, with a second area of higher relative risk in the east, centred on Louth, Meath, Dublin, Newry and Mourne and Down (Map 5.2). There were some smaller areas of higher risk in Waterford, Wexford, Mayo and Derry.
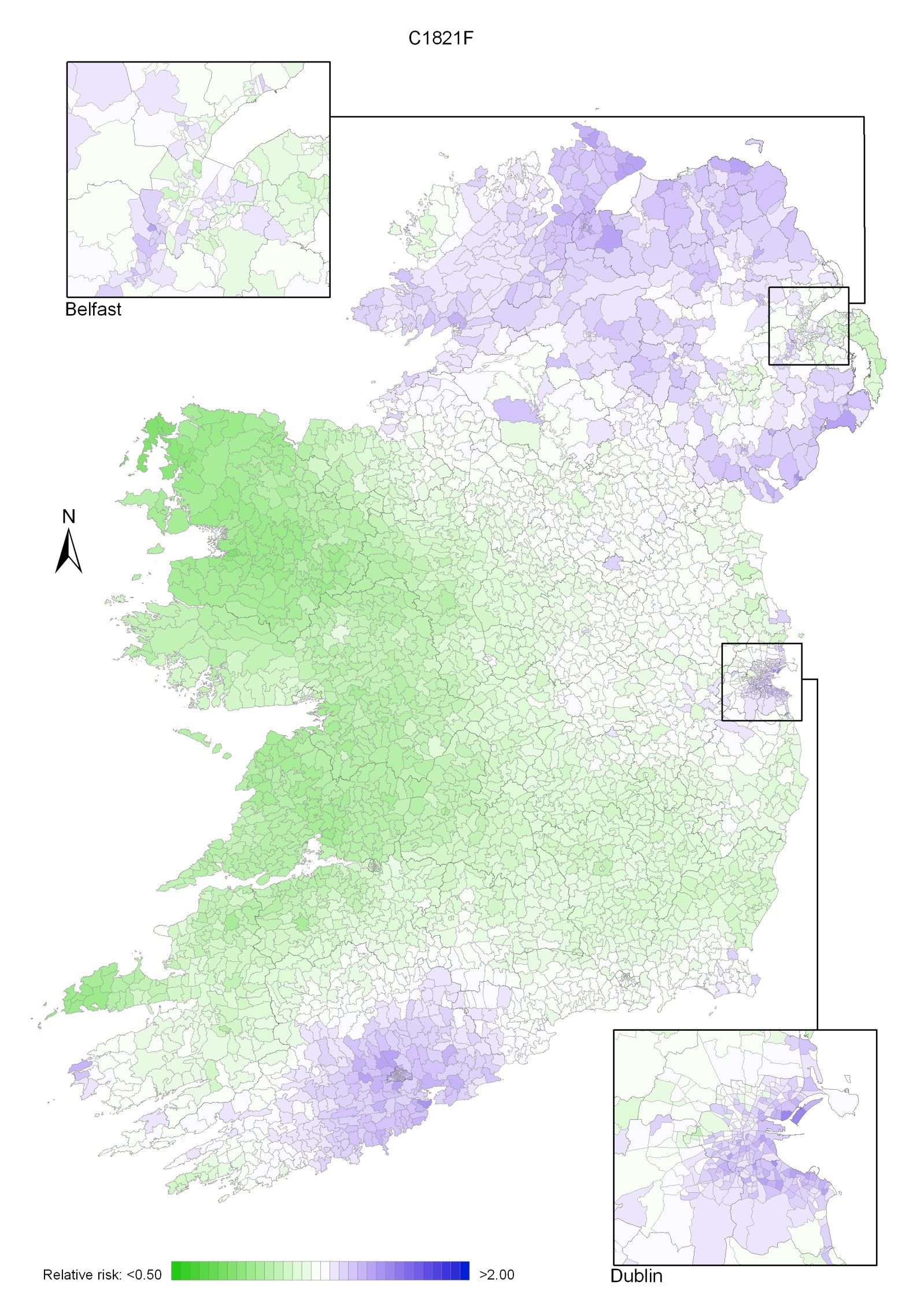
For women, areas of higher risk were principally in the north between east Donegal and north-east Louth, as well as in Dublin city and in Cork city and surrounds. Areas of low relative risk were mostly located in the west (Map 5.3).
Map 5.1 Colorectal cancer, smoothed relative risks: both sexes
Map 5.2 Colorectal cancer, smoothed relative risks: males
Map 5.3 Colorectal cancer, smoothed relative risks: females