Prostate cancer was the most common cancer in men, accounting for 23% of all malignant neoplasms, excluding non-melanoma skin cancer, in men in Ireland (Table 7.1). The average number of new cases diagnosed each year was 2,550. Between 1995 and 2007, the number of new cases more than doubled, increasing by approximately 7% per annum. From 1995 to 2001, the number of new cases diagnosed per annum rose by approximately 9% in RoI and by 2% in NI. From 2002 to 2007 the annual increase was 5% in RoI and 6% in NI.
The risk of developing prostate cancer up to the age of 74 was 1 in 13 and was higher in RoI than in NI. At the end of 2008, 5,235 males aged under 65 and 17,829 aged 65 and over were alive up to 15 years after their prostate cancer diagnosis.
Table 7.1 Summary information for prostate cancer in Ireland, 1995-2007
Ireland | RoI | NI | |
% all new cancer cases | 17% | 18% | 14% |
% all new cancer cases excluding non-melanoma skin cancer | 23% | 25% | 19% |
average number of new cases per year 1995-2007 | 2550 | 1900 | 649 |
average number of new cases per year 1995-2001 | 1955 | 1439 | 517 |
average number of new cases per year 2002-2007 | 3243 | 2439 | 804 |
cumulative risk to age 74 | 8.0% | 8.9% | 6.0% |
15-year prevalence (1994-2008) | 23064 | 17430 | 5634 |
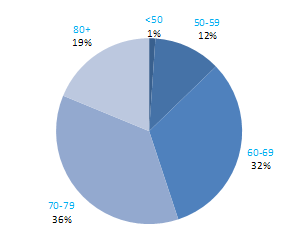
Prostate cancer is predominantly a disease of old age. Just over 1% of cases presented in those aged under 50, while 87% occurred in those aged 60 and older (Figure 7.1). Age at diagnosis was slightly older in NI than in RoI, with 60% aged 70 and over at diagnosis in NI compared with 53% in RoI.
Figure 7.1 Age distribution of prostate cancer cases in Ireland, 1995-2007
Considerable variation exists in prostate cancer incidence rates among developed countries. Estimates for 2008 ranged from 105 per 100,000 men in Australia to 23 per 100,000 in Japan (Figure 7.2). The rate in RoI was in the upper third of the range, while that in NI was in the lower third.
Figure 7.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: prostate cancer
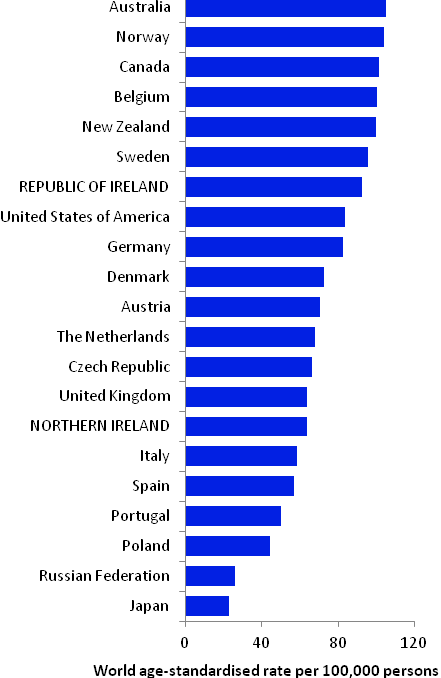
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from cancer registry data for 2005-2007)
Table 7.2 Risk factors for prostate cancer, by direction of association and strength of evidence
Increases risk | Decreases risk | |
Convincing or probable | Family history of prostate cancer1,2 | Foods containing lycopene8,9 |
| Height/tallness3 | |
| Arsenic and arsenic compounds4 | |
| Cadmium and cadmium compounds4 | |
Possible | Obesity (aggressive prostate cancer)5 | Obesity (non-aggressive prostate cancer)5 |
Tobacco smoking6 | Selenium or foods containing selenium9,10 | |
Insulin-like growth factor-1 (IGF-1)7 | Soya and soya food products11,12 | |
Aspirin and other non-steroidal anti-inflammatory drugs13 | ||
| ||
1 One or more relative(s) with prostate cancer; 2 Bruner et al., 2003; 3 Zuccolo et al., 2008; 4 Straif et al., 2009; 5 Giovannucci and Michaud, 2007; 6 Huncharek et al., 2010; 7 Rowlands et al., 2009; 8 lycopene is a carotenoid found in tomatoes and tomato products, such as soup and puree; 9 World Cancer Research Fund / American Institute of Cancer Research, 2007; 10 Jiang et al., 2010; 11 Hwang et al., 2009; 12 Yan and Spitznagel, 2009; 13 Mahmud et al., 2010 | ||
The chances of a man developing prostate cancer are approximately doubled if he has a relative with the disease. Despite extensive study, relatively few other risk factors for prostate cancer have been firmly established (Table 7.2). Taller men appear to have higher risk, although height per se is unlikely to affect a man’s chances of developing the cancer: instead it probably points to relevant childhood exposures. One possibility is that the association operates through the insulin-like growth factor system, which plays a key role in cell proliferation, differentiation and apoptosis. Positive associations have been reported between prostate cancer and circulating levels of insulin-like growth factor 1.
There is limited evidence that exposure to arsenic and inorganic arsenic compounds (through occupational inhalation or ingestion in food or drinking water) and cadmium and cadmium compounds (via occupational use), are a cause of prostate cancer.
Some aspects of diet may influence risk. Higher intake of the carotenoid lycopene is associated with decreased risk in many studies. Risk may be reduced in men, especially those from Asian populations, who consume more tofu and soya food products. While observational studies suggest that higher intake of selenium or selenium-rich foods is also inversely associated with prostate cancer, two trials found no effect of selenium supplementation.
Obesity may be associated with reduced risk of non-aggressive prostate cancer but, since the opposite has been suggested for aggressive disease, the observations could be due to a detection bias relating to the ability to detect prostate cancer in obese men (Buschemeyer and Freedland, 2007). While current smoking per se does not appear to be associated with risk, risk may be elevated among smokers with higher levels of exposure. Meta-analyses suggest the possibility that regular use of aspirin and other non-steroidal anti-inflammatory drugs could be associated with reduced risk of prostate cancer overall, and of advanced cancers specifically, but there are inconsistencies and limitations in the evidence.
Figure 7.3 Adjusted relative risks (with 95% confidence intervals) of prostate cancer by socio-economic characteristics of geographic area of residence | |
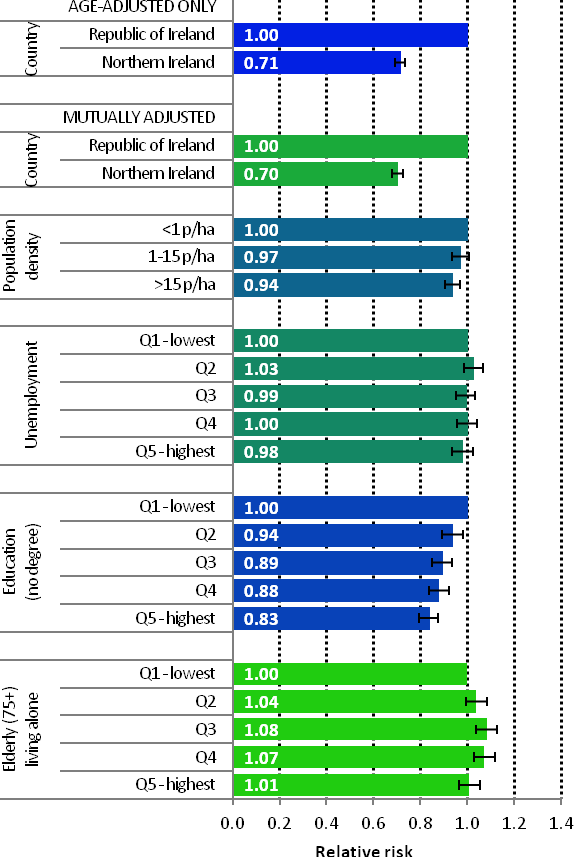 | The risk of prostate cancer in NI was 29% lower than in RoI, with variations between the two countries with regard to socio-economic factors and population density having a minimal impact on this difference (Figure 7.3). There was a weak relationship between prostate cancer and population density, with men living in the least densely populated areas at greater risk. Unemployment was not associated with prostate cancer risk. The strongest area-based factor in prostate cancer risk was education; men resident in areas with a smaller proportion of people with degree level qualifications had a 17% reduced risk compared to those living in areas with the highest proportion of people with degree level qualifications. Men resident in the 3rd and 4th quintiles of the proportion of elderly people living alone indicator had the highest risk of prostate cancer. |
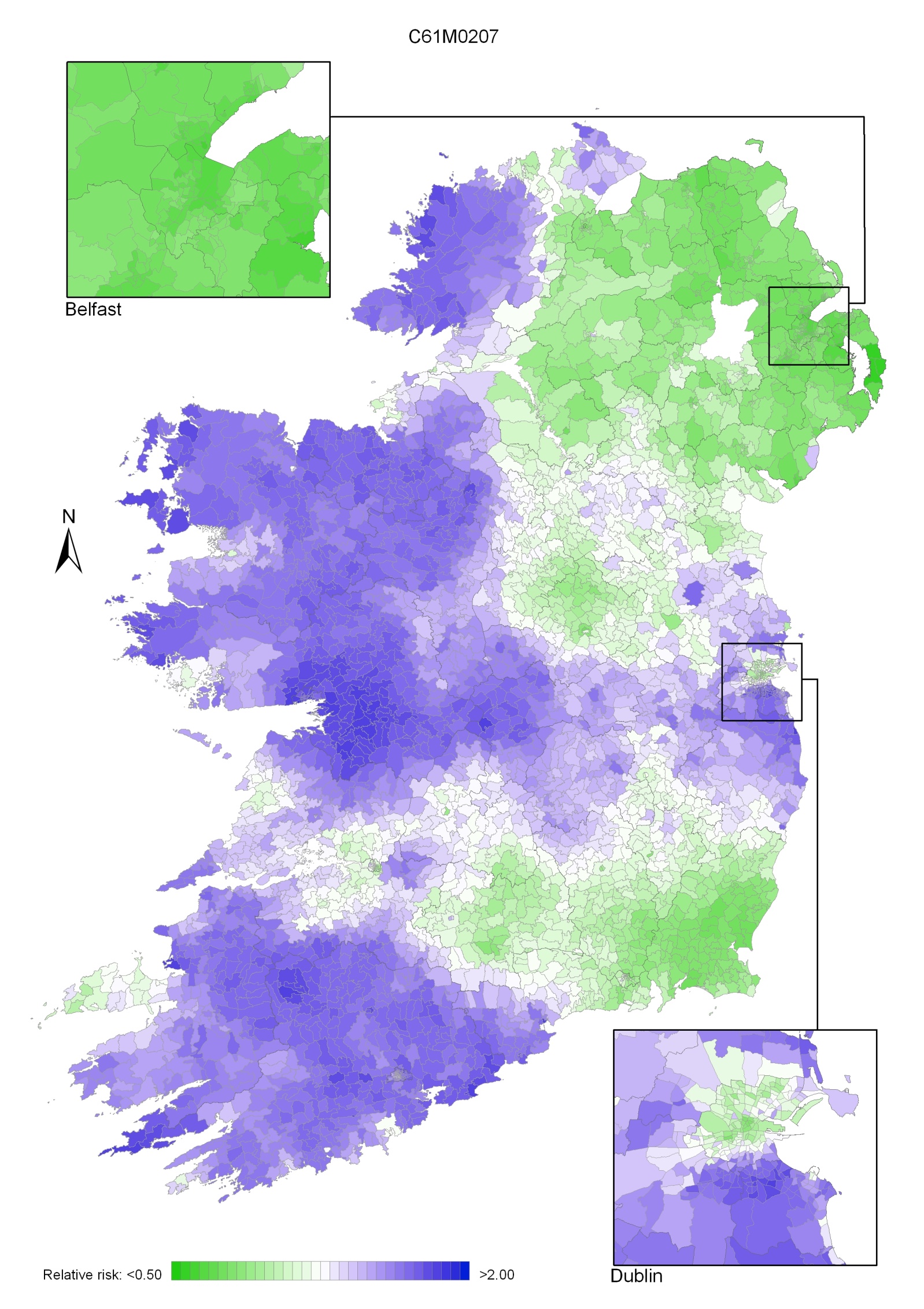
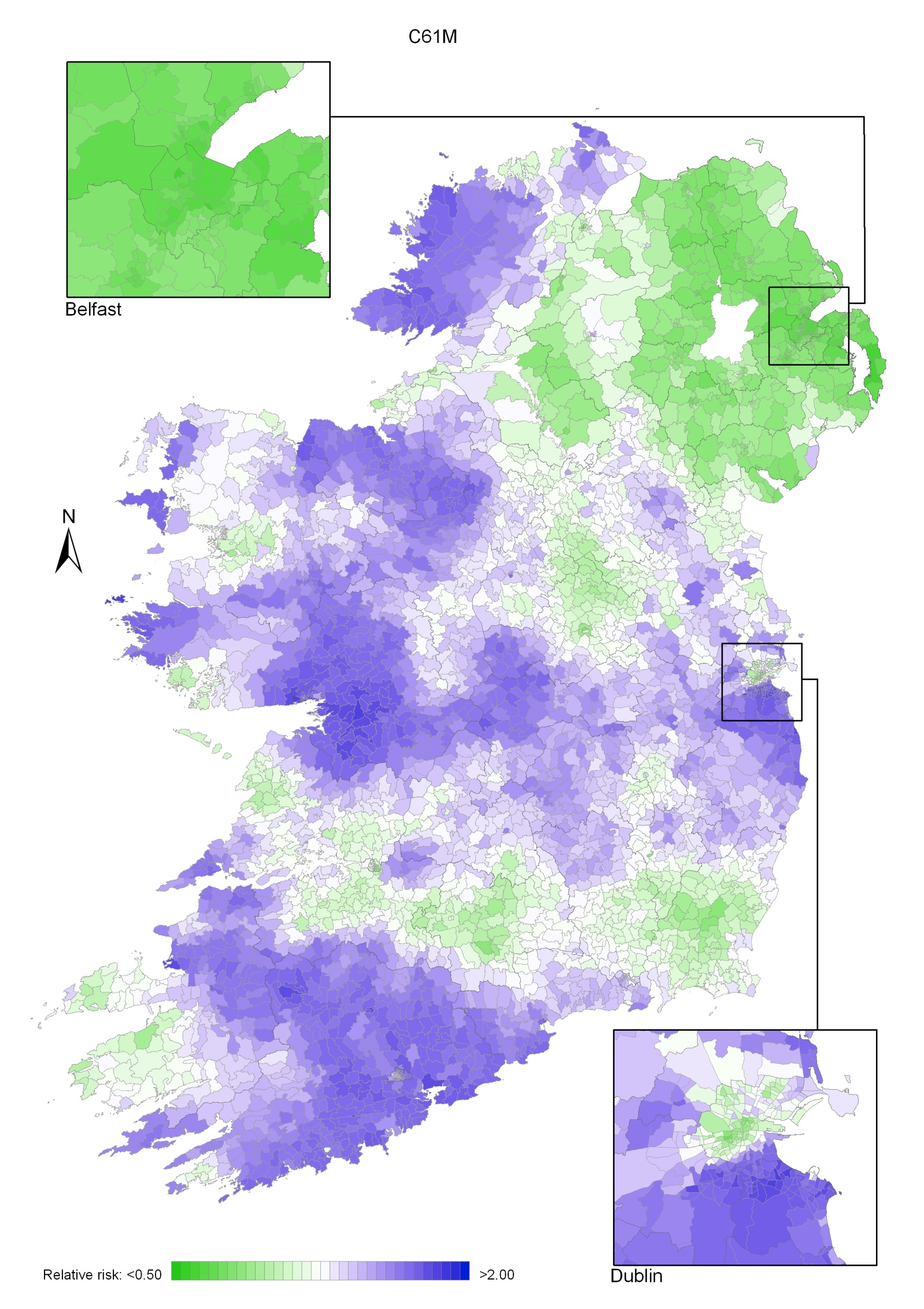
For the period 1995-2007, prostate cancer exhibited a strong geographical pattern with a number of discrete areas of higher risk, mainly in the west.
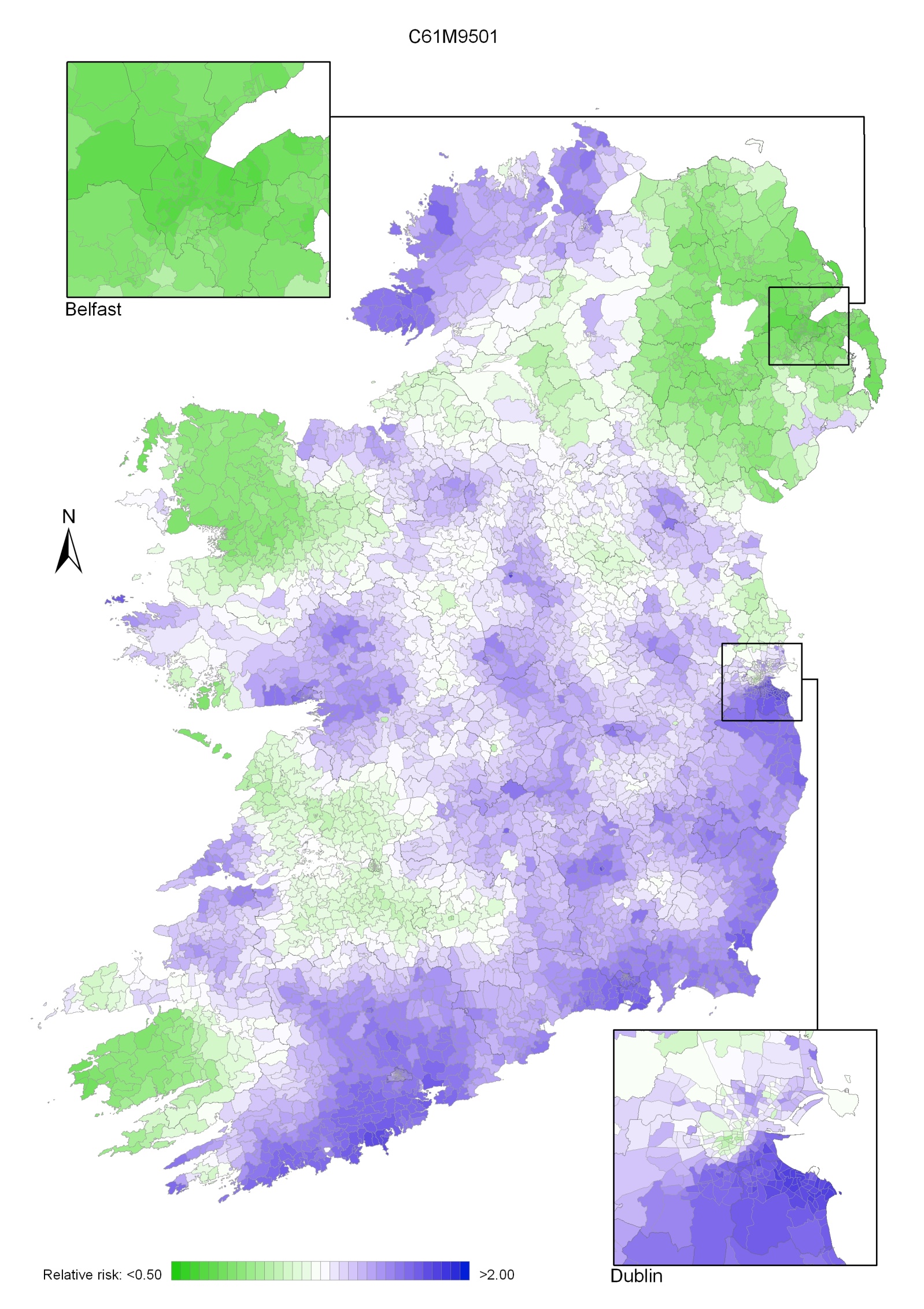
For all time periods, relative risk was lower in NI than in RoI (Map 7.1).
During 1995-2001, the relative risk tended to be higher in the south and east of Ireland. Areas of higher risk were also found in Donegal, Sligo, Galway, Clare and north Kerry (Map 7.2).
During 2002-2007 risk tended to be higher in a number of areas in the west and north-west, including Donegal and across the midlands to the east coast (Map 7.3). Risk was higher in the south of Dublin city compared to the central and northern parts.
Map 7.1 Prostate cancer, smoothed relative risks: 1995-2007
Map 7.2 Prostate cancer, smoothed relative risks: 1995-2001
Map 7.3 Prostate cancer, smoothed relative risks: 2002-2007