9. Stomach cancer
9.1 Summary
Stomach cancer was the sixth most common cancer in Ireland, accounting for 2.7% of all malignant neoplasms, excluding non-melanoma skin cancer, in women and 4.0% in men (Table 9.1). The average number of new cases diagnosed each year was 278 in women and 442 in men. During 1995-2007, the number of new cases diagnosed per annum remained fairly constant.
The risk of developing stomach cancer up to the age of 74 was 1 in 161 for women and 1 in 74 for men and was similar in NI and RoI for both men and women. At the end of 2008, 197 women and 323 men aged under 65, and 522 women and 773 men aged 65 and over, were alive up to 15 years after their stomach cancer diagnosis.
Table 9.1 Summary information for stomach cancer in Ireland, 1995-2007
Ireland | RoI | NI | ||||
females | males | females | males | females | males | |
% of all new cancer cases | 2.0% | 2.9% | 1.9% | 2.7% | 2.1% | 3.3% |
% of all new cancer cases excluding non-melanoma skin cancer | 2.7% | 4.0% | 2.6% | 3.9% | 2.8% | 4.4% |
average number of new cases per year | 278 | 442 | 181 | 294 | 97 | 148 |
cumulative risk to age 74 | 0.6% | 1.4% | 0.6% | 1.3% | 0.6% | 1.4% |
15-year prevalence (1994-2008) | 719 | 1096 | 476 | 746 | 243 | 350 |
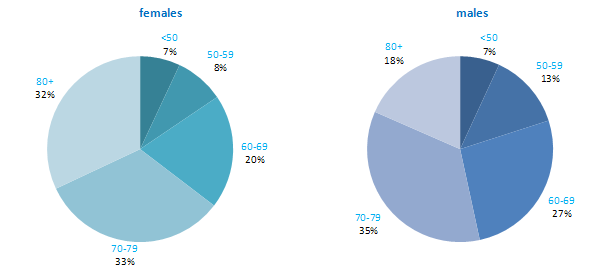
More than 50% of all cases of stomach cancer were diagnosed at over 70 years of age—65% of women and 53% of men (Figure 9.1). Only 7% of cases were aged under 50 years at diagnosis. Patterns were similar for RoI and NI, but with a slightly older age at diagnosis in NI.
Figure 9.1 Age distribution of stomach cancer cases in Ireland, 1995-2007, by sex
9.2 International variations in incidence
Rates of stomach cancer among men and women were considerably higher in Japan than in other developed countries. Within Europe, Russia had the highest incidence rate (Figure 9.2). In RoI and NI rates were moderate compared to other countries for both men and women. Sweden, USA and Canada had particularly low rates of this cancer.
Figure 9.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: stomach cancer | |
| females | males |
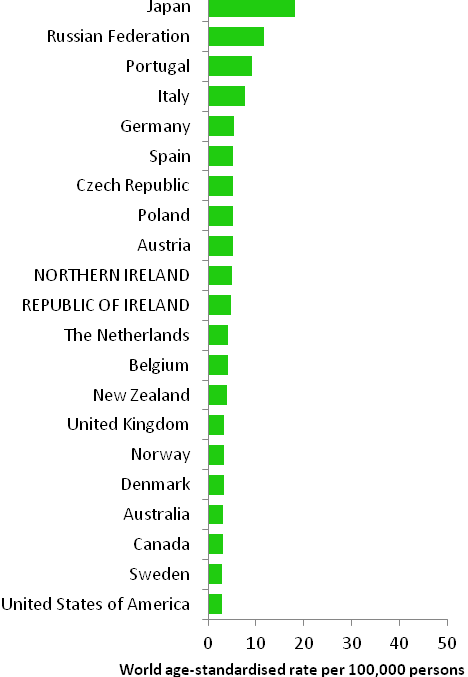 | 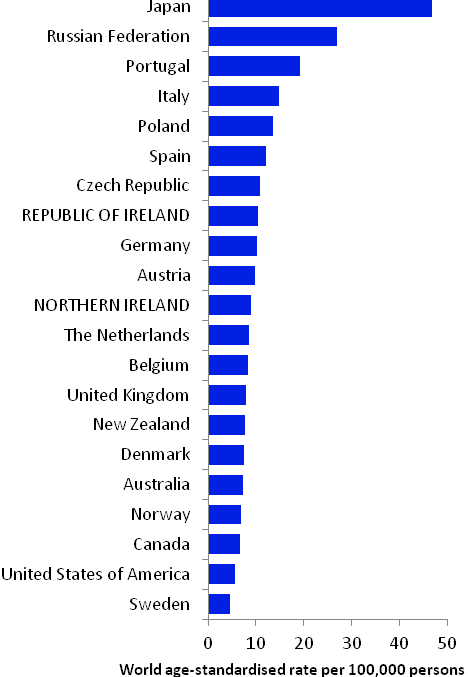 |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from Cancer Registry data for 2005-2007). | |
9.3 Risk factors
Table 9.2 Risk factors for stomach cancer, by direction of association and strength of evidence
Increases risk | Decreases risk | |
Convincing or probable | Helicobacter pylori infection1 | Non-starchy and fresh vegetables4,8,10 |
| Epstein-Barr virus2 | Fruit4,10 |
| Tobacco smoking3 | Refrigeration4 |
| Salt, salted and salty foods, or salt preserved foods, including Chinese-style salted fish3,4 | Aspirin and other non-steroidal anti-inflammatory drugs11,12 |
| Ionizing radiation5 | |
| Low socio-economic status6 | |
Possible | Fermented soya foods7 | Non-fermented soya foods7 |
Pickled vegetables8 | ||
Overweight/obesity9 | ||
1 Helicobacter and Cancer Collaborative Group, 2001; 2 International Agency for Research on Cancer, 2011b; 3 Secretan et al., 2009; 4 World Cancer Research Fund / American Institute for Cancer Research, 2007; 5 El Ghissassi et al., 2009; 6 Faggiano et al., 1997; 7 Kim et al., 2011; 8 Kim et al., 2010; 9 Yang et al., 2009; 10 International Agency for Research on Cancer, 2003; 11 Tian et al., 2010; 12 Yang et al., 2010 | ||
Infection with the common bacterium, Helicobacter pylori (H pylori), which lives in the stomach and causes inflammation and ulcers, is associated with a six-fold raised risk of stomach cancer (Table 9.2). Meta-analysis of intervention studies shows that stomach cancer risk is decreased by one-third in H pylori-positive patients randomised to eradication treatment (Fuccio et al., 2009). It has been suggested that H pylori infection may be a necessary (but not sufficient) cause of cancers in the distal stomach (International Agency for Research on Cancer, 1994). It is also probable that infection with the Epstein-Barr virus (EBV), which is a member of the herpesvirus family, and very common, is a cause of stomach cancer.
Smoking is firmly established as a cause of stomach cancer. Compared to non-smokers, risk in increased by 50% in those who have ever smoked and 70% in current smokers (La Torre et al., 2009). Risk also increases with number of cigarettes smoked (Ladeiras-Lopes et al., 2008). Those with low socio-economic status have increased stomach cancer risk, probably in part reflecting variations in tobacco use by social class.
Other than these factors, the main risk factors are related to food and food preservation. There is substantial and consistent evidence that higher intakes of salt, salty foods or foods preserved in salt are associated with increased risk. Risk is reduced in individuals with higher intakes of fruit and non-starchy or fresh vegetables; in contrast there may be a modest increased risk in those who consume higher quantities of pickled vegetables. More than 10 studies have reported a significant reduction in disease risk with use of refrigeration. However, it is thought that the association is not due to refrigeration per se but rather is a consequence of other factors related to refrigerator use, such as lower intake of foods preserved with salt, or higher intake of fresh perishable foods (e.g. vegetables and fruit) (World Cancer Research Fund / American Institute for Cancer Research, 2007).
In terms of other potential risk factors, use of aspirin and other non-steroidal anti-inflammatory drugs has been associated with a modest (approximately 20%) reduction in risk of stomach cancer; this association appears stronger after adjusting for other risk factors. Overweight individuals (body mass index >25kg/m2) may have a modest increased risk, particularly for cancers arising in the gastric cardia.
9.4 Small geographic area characteristics and cancer risk
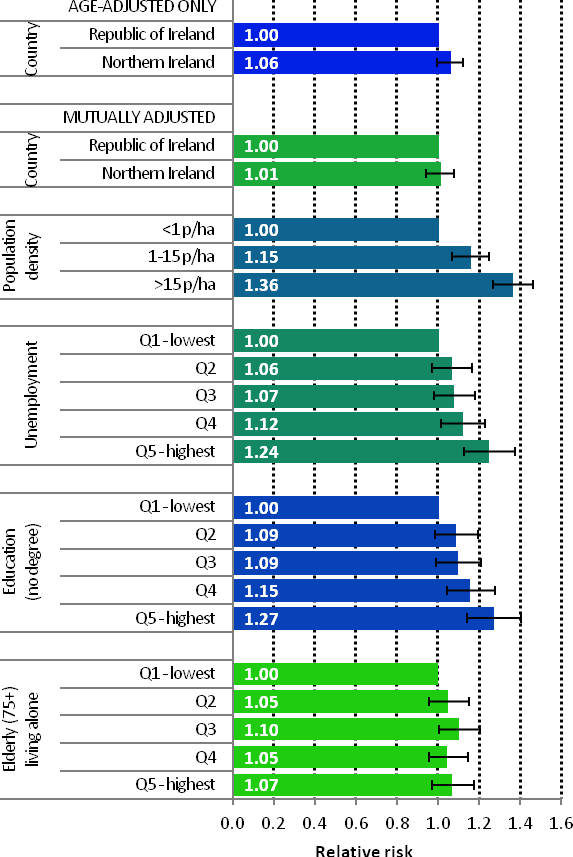
Figure 9.3 Adjusted relative risks (with 95% confidence intervals) of stomach cancer by socio-economic characteristics of geographic area of residence: males
| MalesDifferences in male stomach cancer risk between RoI and NI were not statistically significant, either when adjusted for age, or when adjusted for age, population density and socio-economic factors (Figure 9.3). Male stomach cancer risk varied by area-based characteristics. Men resident in areas with 1-15 p/ha had a 15% greater risk of stomach cancer than those resident in the least densely populated areas, while those resident in the most densely populated areas had a 36% greater risk. Stomach cancer risk increased as the proportion of unemployed in an area increased. The same pattern was seen for educational attainment; people living in areas with low levels of educational attainment had the greatest risk of stomach cancer. There was no consistent association of risk with the percentage of people aged 75 and over living alone. |
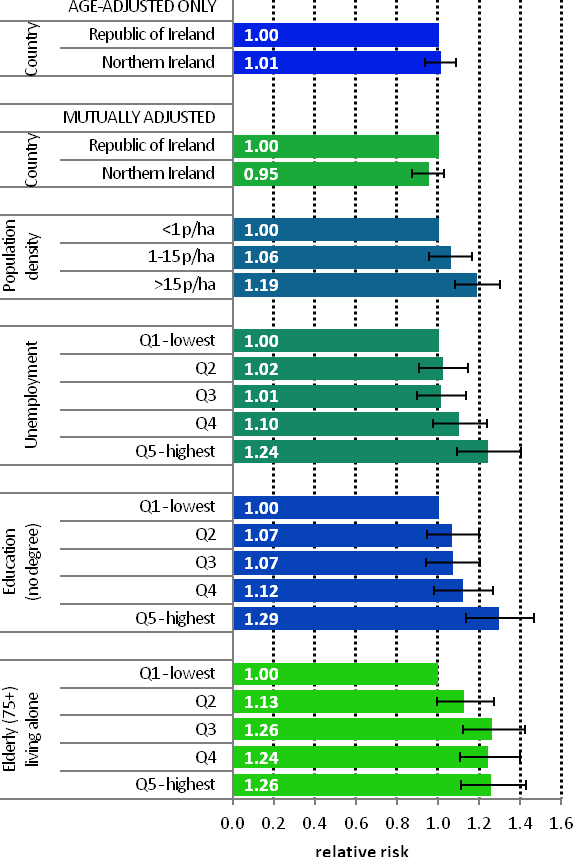
Figure 9.4 Adjusted relative risks (with 95% confidence intervals) of stomach cancer by socio-economic characteristics of geographic area of residence: females
| FemalesThe pattern for women was very similar to that for men (Figure 9.4). There was no significant difference between countries, but stomach cancer risk increased with increasing levels of unemployment, lower educational attainment and population density. The relationship between female stomach cancer risk and areas where there were higher levels of elderly people living alone was stronger than that for men. Compared to areas with low levels of elderly people living alone, the relative risk of stomach cancer in areas with the highest proportion of elderly people living alone was 1.26 (95%CI=1.11-1.43). Quintiles 3 and 4 also had similar levels of increased risk. |
9.5 Mapping and geographical variation
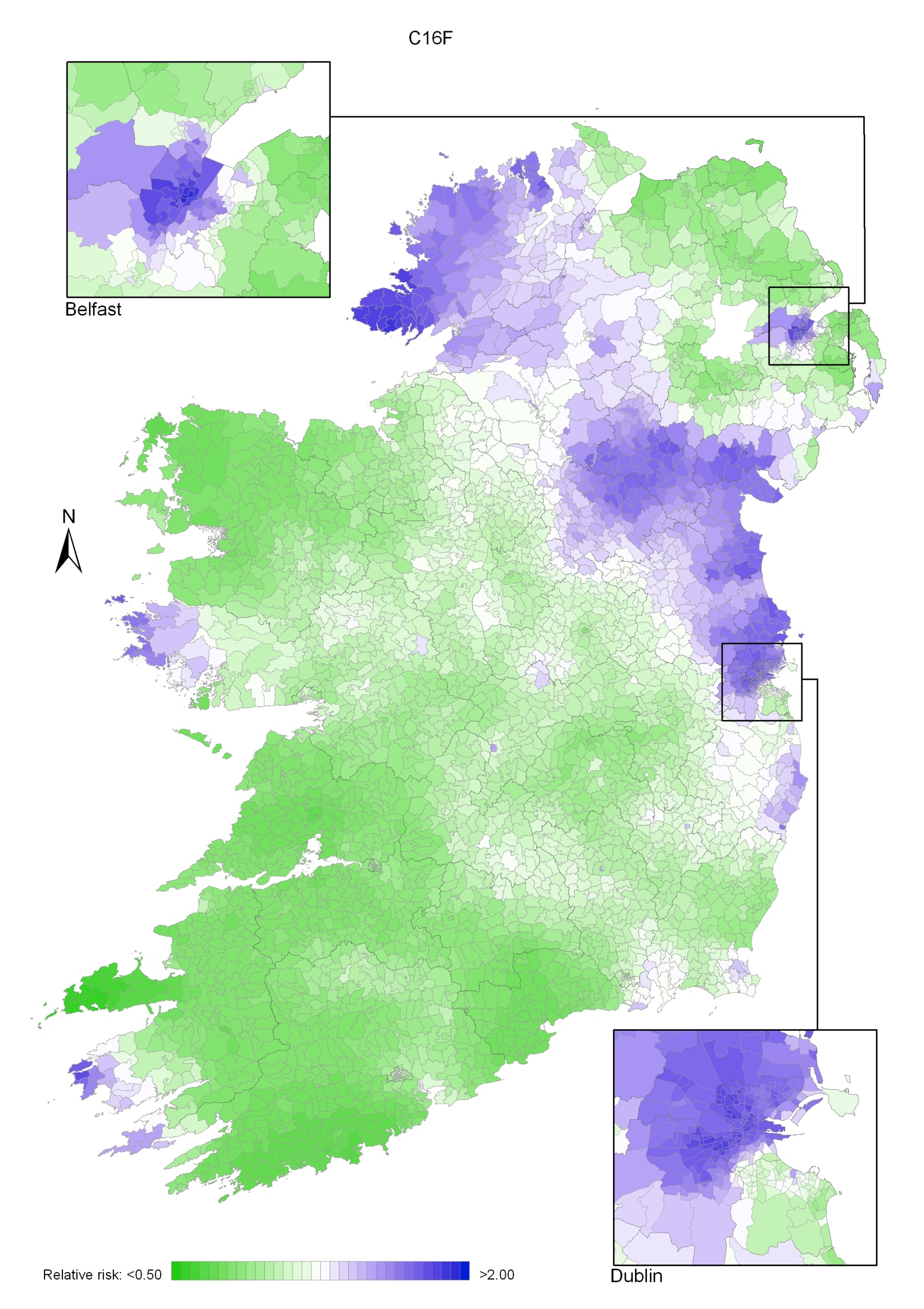
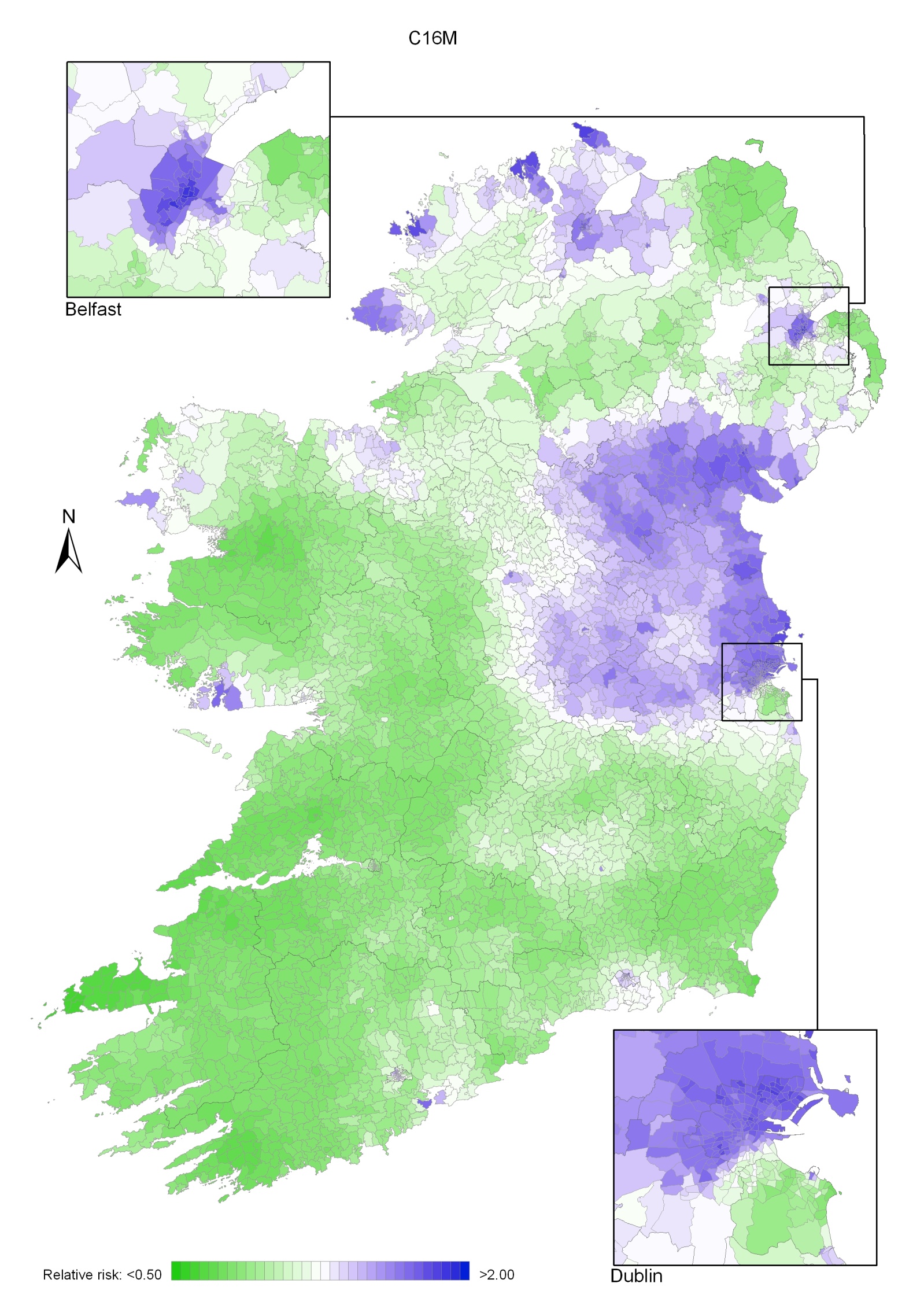
Stomach cancer had a strong geographical pattern with lower relative risk in most of the south and west of Ireland and higher relative risk in parts of the north (Maps 9.1-9.3).
For both sexes combined, the main area of higher relative risk extended northwards from Dublin as far as the border counties and west into the midlands (Map 9.1). There were also isolated areas of higher risk in Donegal, Belfast, Antrim, north Lisburn, Kerry and Connacht.
The pattern for men was similar to that for both sexes combined (Map 9.2).
For women, the main area of higher relative risk extended in a band from Dublin to Donegal, excluding the north-east of NI, but including Belfast, south Antrim, north Lisburn, Ards and parts of Down. Comparatively high relative risk was also found in western parts of Galway, west Cork and west Kerry (Map 9.3).
Map 9.1 Stomach cancer, smoothed relative risks: both sexes
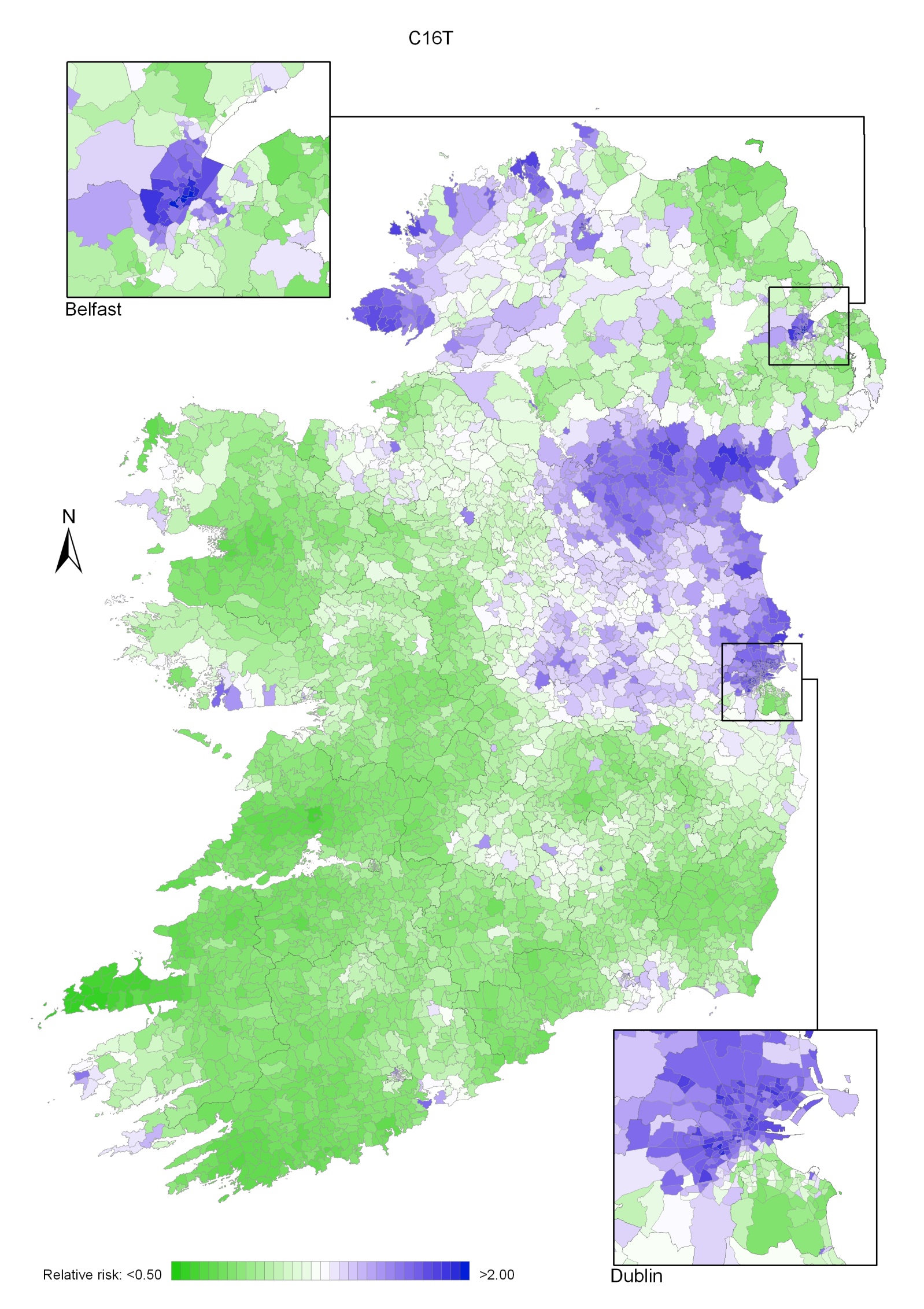
Map 9.2 Stomach cancer, smoothed relative risks: males
Map 9.3 Stomach cancer, smoothed relative risks: females