Melanoma of the skin was the seventh most common cancer in Ireland, accounting for 4.1% of all malignant neoplasms, excluding non-melanoma skin cancer, in women and 2.6% in men (Table 10.1). The average number of new cases diagnosed each year was 421 in women and 285 in men. During 1995-2007, the number of new cases diagnosed increased at approximately 5% per annum overall.
The risk of developing melanoma up to the age of 74 was 1 in 89 for women and 1 in 116 for men, and was slightly higher in RoI than in NI. At the end of 2008, 2,991 women and 1,707 men aged under 65, and 2,140 women and 1,336 men aged 65 and over, were alive up to 15 years after their melanoma diagnosis.
Table 10.1 Summary information for melanoma of the skin in Ireland, 1995-2007
Ireland | RoI | NI | ||||
females | males | females | males | females | males | |
% of all new cancer cases | 3.0% | 1.9% | 3.1% | 1.9% | 2.7% | 1.8% |
% of all new cancer cases excluding non-melanoma skin cancer | 4.1% | 2.6% | 4.3% | 2.6% | 3.6% | 2.5% |
average number of new cases per year | 421 | 285 | 298 | 201 | 123 | 84 |
cumulative risk to age 74 | 1.1% | 0.9% | 1.2% | 0.9% | 1.0% | 0.8% |
15-year prevalence (1994-2008) | 5131 | 3043 | 3525 | 2074 | 1606 | 969 |
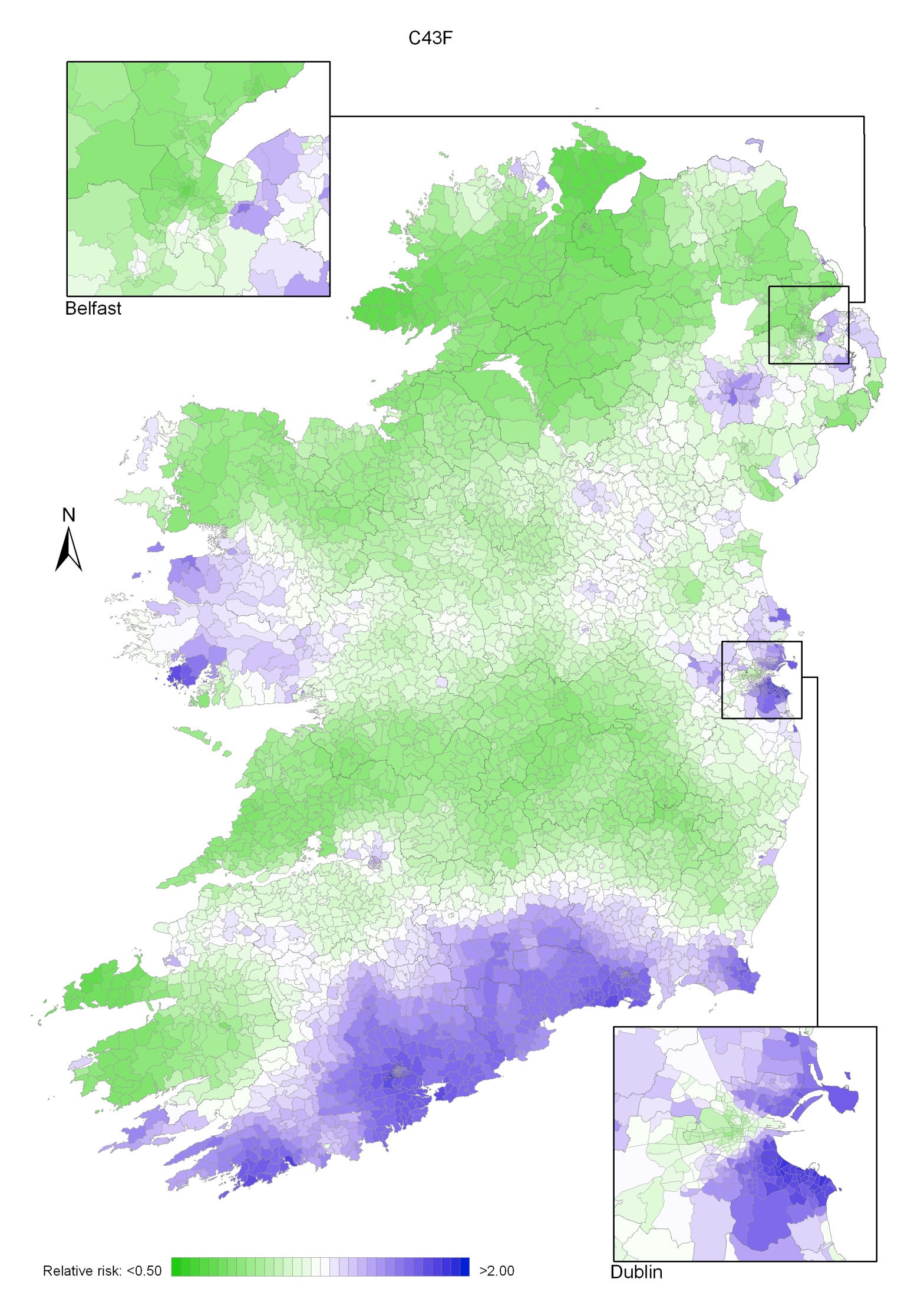
Melanoma of the skin is a disease of younger age groups, with 36% of women and 31% of men aged under 50 at diagnosis (Figure 10.1). Over half of all new cases presented under 60 years. However, a substantial proportion of cases (12-13%) was diagnosed in the age group 80 and older. Age patterns were similar for RoI and NI.
Figure 10.1 Age distribution of cases of melanoma of the skin in Ireland, 1995-2007, by sex
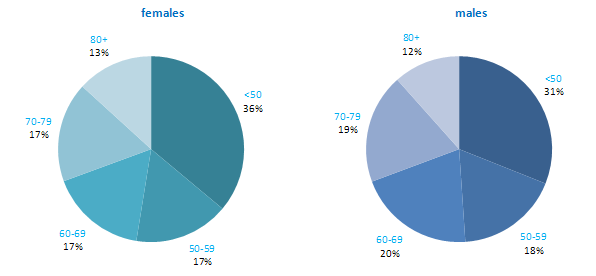
For both men and women Australia and New Zealand had the highest incidence rates of melanoma, while Japan had the lowest (Figure 10.2). Both RoI and NI had moderate rates of melanoma compared to other developed countries. Rates in both parts of Ireland were lower than in the UK.
Figure 10.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: malignant melanoma of skin | |
| females | males |
 |  |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from Cancer Registry data for 2005-2007). | |
Table 10.2 Risk factors for melanoma of the skin, by direction of association and strength of evidence
| Increases risk | Decreases risk |
Convincing or probable | Sun exposure (mainly recreational)1-3 | |
| Sunbed/sunlamp use4 | |
| History of sunburn1-3,5 | |
| Presence of benign sun damage in the skin2,5 | |
| Number of naevi2,6,7 | |
| Density of freckles or freckling as a child2,8 | |
| Skin, hair and eye colour1,2,8,9 | |
| Ability to tan2 | |
| Family history of melanoma8,10,11 | |
| High socio-economic status12 | |
Possible | Body fatness and weight gain in adulthood13,14 | |
1 International Agency for Research on Cancer, 2001; 2 Armstrong and Kricker, 2001; 3 Gandini et al., 2005a; 4 El Ghissasi et al., 2009; 5 Olsen et al., 2011; 6 risk raised for high numbers of either common or atypical naevi or both; 7 Olsen et al., 2010b; 8 Gandini et al., 2005b; 9 Olsen et al., 2010b; 10 Olsen et al., 2010c; 11 melanoma in one or more first degree relatives; 12 Faggiano et al., 1997; 13 Olsen et al., 2008; 14 Renehan et al., 2008 | ||
Exposure to ultraviolet (UV) radiation, the primary source of which is sunlight, is the main cause of melanoma of the skin (Table 10.2). Risk increases with increasing levels of intermittent, or recreational, sun exposure. A history of sunburn, often considered to be a marker of high levels of intermittent sun exposure, is associated with raised risk in a dose-response fashion. Presence of benign sun damage (solar keratoses) is a marker of increased risk, particularly for melanomas on the head and neck. Exposure to artificial UV radiation, through use of sunbeds or sunlamps, also causes melanoma. Constitutional factors act together with UV exposure to influence the chance of an individual developing melanoma. Risk is increased in those with more naevi (moles), a high density of freckles (or who had freckling as a child), light hair, skin or eye colour, and less ability to tan.
Melanoma risk is higher in those of higher socio-economic status. This may be due to greater recreational sun exposure among more affluent groups.
Individuals with one or more first degree relatives who have had melanoma have a two-fold increased risk of developing it themselves. On average, around 4% of cases of melanoma are estimated to be attributable to familial risk.
In terms of more tentative associations, modest positive relationships have been reported between melanoma risk and higher body mass index in men and weight gain in adulthood in women.
Figure 10.3 Adjusted relative risks (with 95% confidence intervals) of melanoma of the skin by socio-economic characteristics of geographic area of residence: males
| MalesThe relative risk of melanoma of the skin among men was 8% lower in NI than in RoI (Figure 10.3). Once differences in population density and socio-economic factors were adjusted for, this difference increased to 15%. Areas with average (1-15 p/ha) population density had a 20% greater risk of male melanoma than the least densely populated areas. Areas with the highest levels of unemployment had a reduced risk of melanoma among men. A strong inverse relationship was also present with regard to lower levels of educational attainment in an area. Compared to areas with high levels of tertiary level education, the relative risk of melanoma in areas with low levels of tertiary level education was 0.66 (95%CI = 0.58-0.75). Men resident in areas with between 36% and 42% of elderly people living alone (quintile 4) had an 18% greater risk of melanoma. |
Figure 10.4 Adjusted relative risks (with 95% confidence intervals) of melanoma of the skin by socio-economic characteristics of geographic area of residence: females
| FemalesAmong women, lung cancer risk was higher in NI compared to RoI (RR=1.07, 95%CI=1.01-1.13) (Figure 6.4). However, adjusting for population density and socio-economic factors reversed this relationship, with risk lower in NI (RR=0.92, 95%CI=0.88-0.97). For women the association between lung cancer and population density was greater than for men, with lung cancer risk 74% higher in high density compared to low density areas. Lung cancer among women was higher in areas of high unemployment, lower levels of degree level education and with a high proportion of elderly living alone. The relative risk for people living in areas with the highest proportion of these indicators was 45%, 23% and 9% respectively, compared to the areas with the lowest proportion of these indicators. |
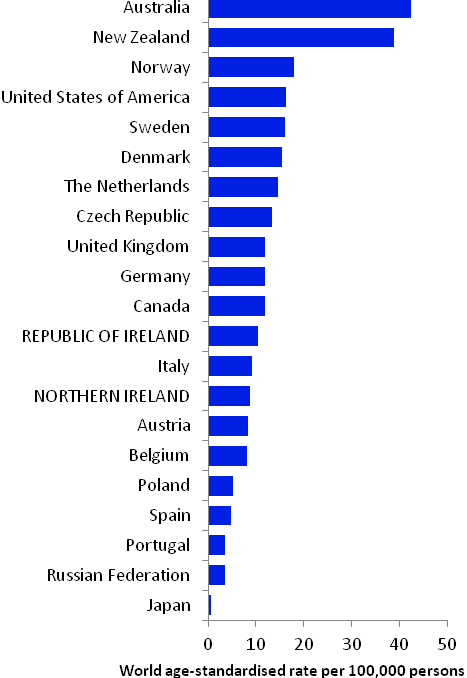
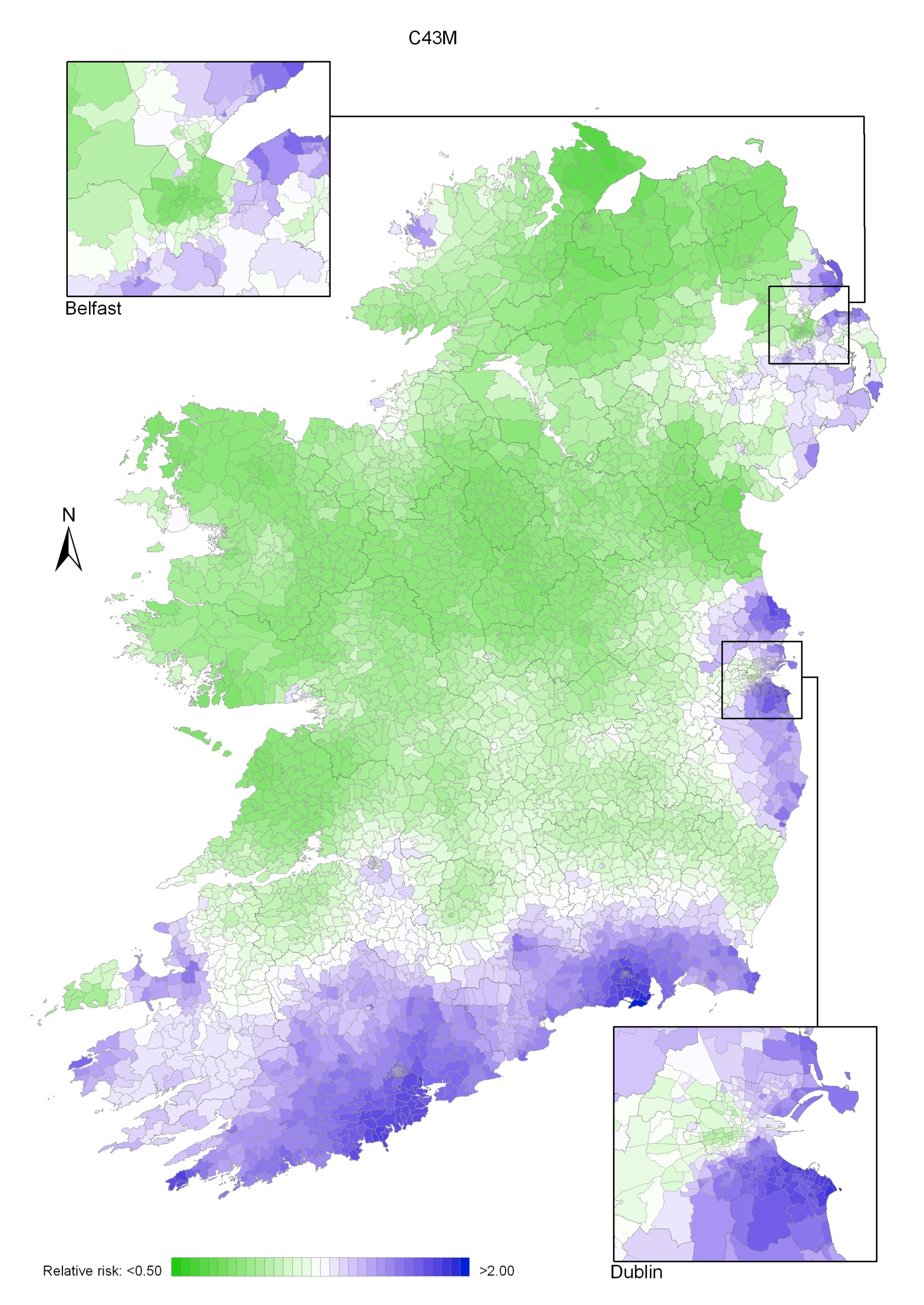
Melanoma of the skin had a strong geographical pattern which was similar for men and women. Areas of higher relative risk were seen along the south coast from Cork to Wexford, and also along the east coast from Meath to Wicklow and in parts of Larne, Castlereagh, Ards, Down, Armagh, Craigavon, Banbridge, Newry and Mourne, Kerry, Limerick, Galway and Mayo (Map 10.1).
The pattern for men was similar to that for both sexes combined (Map 10.2)
For women (Map 10.3) the area of higher risk was slightly more dispersed around Dublin. Areas of higher relative risk were also seen in western parts of Galway and Mayo and in north Leinster.
Map 10.1 Melanoma of the skin, smoothed relative risks: both sexes
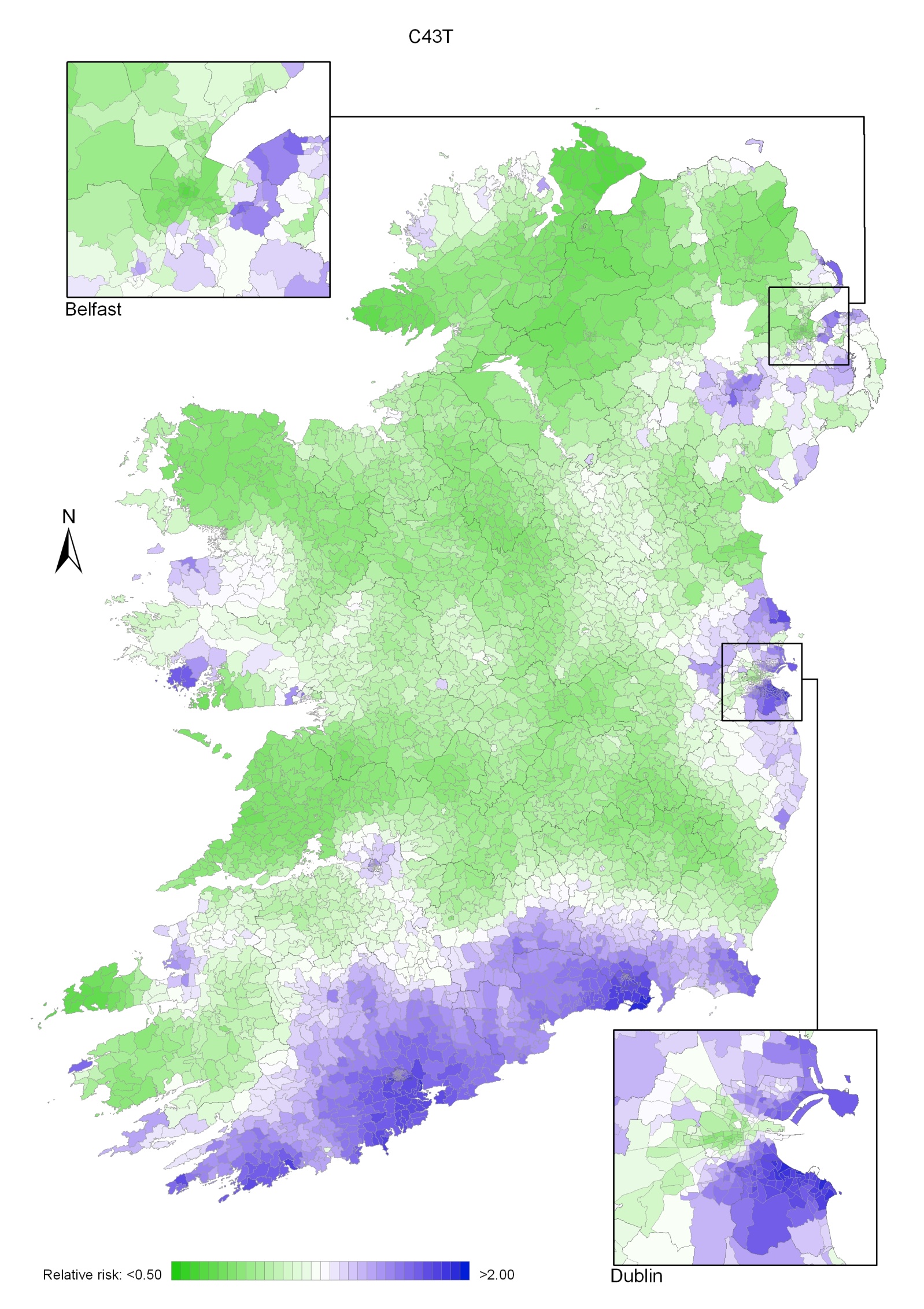
Map 10.2 Melanoma of the skin, smoothed relative risks: males
Map 10.3 Melanoma of the skin, smoothed relative risks: females