Leukaemia describes a number of diseases of differing aetiology and clinical course. The four main subtypes are chronic lymphocytic leukaemia (CLL), chronic myeloid leukaemia (CML), acute lymphocytic leukaemia (ALL) and acute myeloid leukaemia (AML). The commonest of these (about 40% of all cases) is CLL (National Cancer Registry, 2010a). All leukaemias combined formed the tenth most common cancer in Ireland, accounting for 2.4% of all malignant neoplasms, excluding non-melanoma skin cancer, in women and 3.2% in men (Table 13.1). The average number of new cases diagnosed each year was 243 in women and 348 in men. During 1995-2007, the number of new cases diagnosed showed a small overall increase of 1% per annum. However, the numbers decreased slightly in NI, while increasing at approximately 2% per annum in RoI.
The risk of developing leukaemia up to the age of 74 was 1 in 170 for women and 1 in 98 for men and was higher in RoI than in NI. At the end of 2008, 847 women and 1,196 men aged under 65, and 663 women and 924 men aged 65 and over, were alive up to 15 years after their leukaemia diagnosis.
Table 13.1 Summary information for leukaemia in Ireland, 1995-2007
Ireland | RoI | NI | ||||
females | males | females | males | females | males | |
% of all new cancer cases | 1.7% | 2.3% | 1.8% | 2.4% | 1.6% | 2.0% |
% of all new cancer cases excluding non-melanoma skin cancer | 2.4% | 3.2% | 2.5% | 3.4% | 2.1% | 2.8% |
average number of new cases per year | 243 | 348 | 172 | 256 | 71 | 92 |
cumulative risk to age 74 | 0.6% | 1.0% | 0.6% | 1.1% | 0.5% | 0.8% |
15-year prevalence (1994-2008) | 1510 | 2120 | 1115 | 1614 | 395 | 506 |
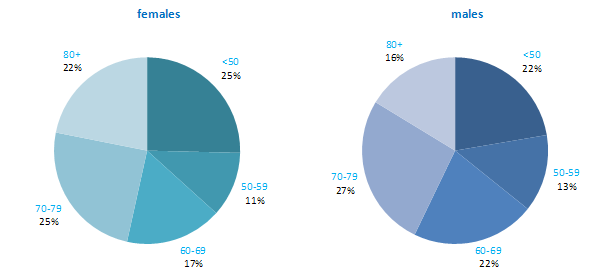
In contrast to most other cancers leukaemia was more common at the extremes of age—47% of women and 38% of men were aged either under 50 or over 79 years at diagnosis (Figure 13.1). Approximately one quarter of all new cases presented in the age group 70–79 years. The pattern of age at diagnosis was similar in RoI and in NI.
Figure 13.1 Age distribution of leukaemia cases in Ireland, 1995-2007, by sex
Leukaemia rates in RoI were relatively high compared with many other developed countries, while rates in NI were relatively low, especially for men (Figure 13.2). New Zealand, USA, Australia and Canada had the highest male rates, while Poland and Japan had the lowest. New Zealand and Italy had the highest female rates of the disease, while Poland and Japan also had the lowest female rates.
Figure 13.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: leukaemia | |
| females | males |
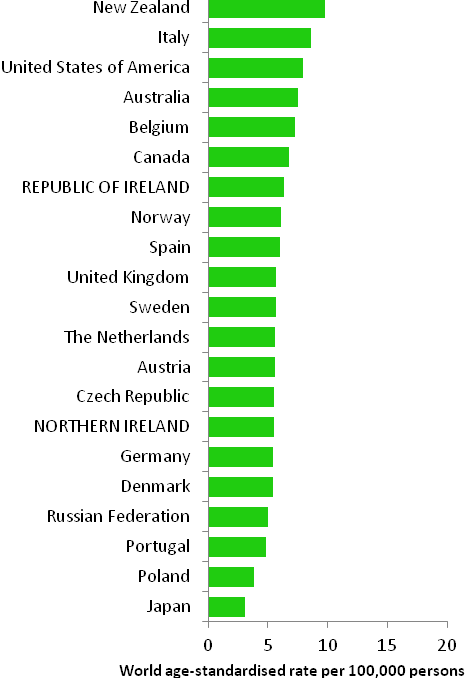 | 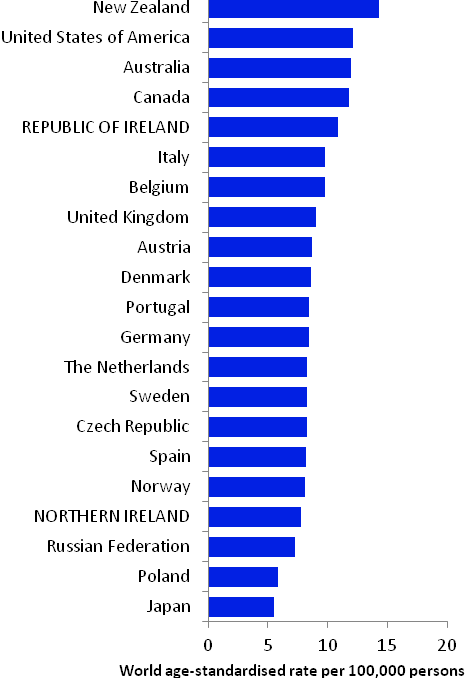 |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from Cancer Registry data for 2005-2007) | |
Table 13.2 Risk factors for leukaemia, by direction of association and strength of evidence
Increases risk | Decreases risk | |
Convincing or probable | Ionizing radiation1,2,3 | |
| Anti-neoplastic drugs4 | |
| Myelodysplastic syndromes5,6 | |
| Human T-cell lymphotrophic virus, type-1 (HTLV-1)7 | |
| Smoking8 | |
| Occupational exposure to formaldehyde, benzene or styrene9,10,11 | |
| Employment in the rubber manufacturing industry9 | |
| Family history of leukaemia12 | |
Possible | Employment in pesticide manufacturing13 | |
Overweight and obesity14,15 | ||
| ||
1 exposure to alpha-particle or beta-particle emitters, x-rays or gamma rays; 2 El Ghissassi et al., 2009; 3 Daniels and Schubauer-Berigan, 2011; 4 International Agency for Research on Cancer, 2011a; 5 conditions of the blood or bone marrow, where individuals have too few of one or more types of healthy blood cells; 6 Garcia-Manero, 2011; 7 International Agency for Research on Cancer, 2011b; 8 Secretan et al., 2009; 9 Baan et al., 2009; 10 Schwilk et al., 2010; 11 National Toxicology Program, 2011; 12 Brown, 2008; 13 Van Maele-Fabry et al., 2008; 14 Larsson and Wolk, 2008; 15 Lichtman, 2010 | ||
The chronic leukaemias (CLL, CML) almost never affect children; AML may affect adults and children; while ALL is the most common type of leukaemia in children, but may affect adults also. The description of risk factors below refers to leukaemia in adults.
Ionizing radiation exposure has long been established as a risk factor for leukaemia. Risk of all types of leukaemia other than CLL is increased in individuals who receive particular types of radiation therapy or undergo multiple x-rays, or have protracted exposure to low-dose gamma radiation. A variety of anti-neoplastic drugs (alkylating agents), given as part of the treatment for other types of cancer, can cause leukaemia, most usually AML. Risk is increased in individuals with myelodysplastic syndrome, a diverse collection of conditions related to the blood and bone marrow which, if left untreated, may progress to AML. Infection with the human T-cell lymphotrophic virus, type 1 (HTLV-1) causes a rare type of leukaemia known as adult T-cell leukaemia. Approximately 10% of individuals with CLL report a family history of the condition or a related lymphoproliferative disorder, but the genes which account for increased susceptibility have not been identified.
Occupational exposure to benzene (an industrial solvent and precursor to basic industrial chemicals including drugs, plastics, synthetic rubber, and dyes); formaldehyde (used in the production of industrial resins that are then used in the manufacture of products such as adhesives and binders for wood products, plastic and synthetic fibres); and styrene (used in the production of polymers, which are incorporated into products such as rubber, plastic, insulation, fibreglass, and car parts) are all linked with leukaemia. Formaldehyde is particularly associated with AML. Workers in the rubber manufacturing industry have increased risk, but due to the complexity of exposures in this industry, the causative agents have not yet been firmly identified. Risk of myeloid leukaemias may also be raised in individuals employed in plants manufacturing pesticides.
In terms of lifestyle-related risk factors, tobacco smoking is a causal agent for myeloid leukaemia. Overweight and obesity may modestly increase risk of all four main subtypes, but the evidence-base is sparse.
Figure 13.3 Adjusted relative risks (with 95% confidence intervals) of leukaemia by socio-economic characteristics of geographic area of residence: males | MalesLeukaemia risk among men was 23% lower in NI than RoI during 1995-2007 (Figure 13.3). Adjustments for different area-based characteristics in each country increased this difference slightly to 25%. There was no association between male leukaemia risk and population density, unemployment or education. Risk increased with an increasing proportion of elderly people in the area living alone. The difference in risk between areas with the least and greatest proportion of elderly people living alone was 17%. |
Figure 13.4 Adjusted relative risks (with 95% confidence intervals) of leukaemia by socio-economic characteristics of geographic area of residence: females
| FemalesLeukaemia risk for women was lower in NI than RoI, by 21% after adjustments for population density and socio-economic factors (Figure 13.4). As for men, there was no association between female leukaemia risk and population density, unemployment or education. The risk of female leukaemia was 14% greater in areas with the greatest proportion of elderly people living alone, compared to areas with the smallest proportion. |
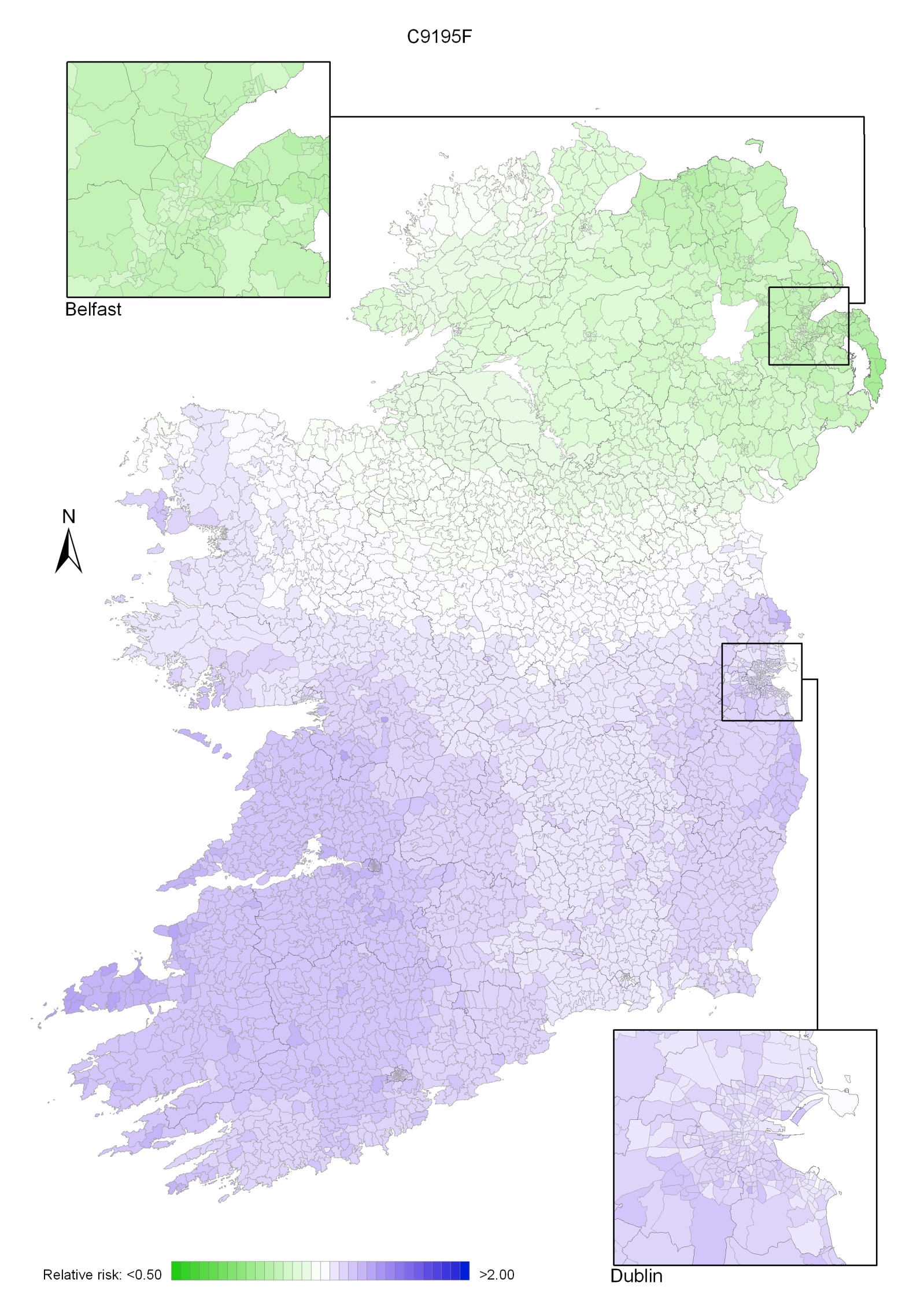
Leukaemia had a very strong geographical pattern of relative risk, which was similar for men and women, although more pronounced in men (Maps 13.1-13.3).
The maps show a gradient of risk across the island, highest in the south-west and reducing uniformly across the country, with the lowest risk in the north-east (Map 13.1).
This pattern was more pronounced for men (Map 13.2) than women (Map 13.3). There was no marked variation in risk within the urban areas, which had similar risks to their surrounding rural areas.
Map 13.1 Leukaemia, smoothed relative risks: both sexes
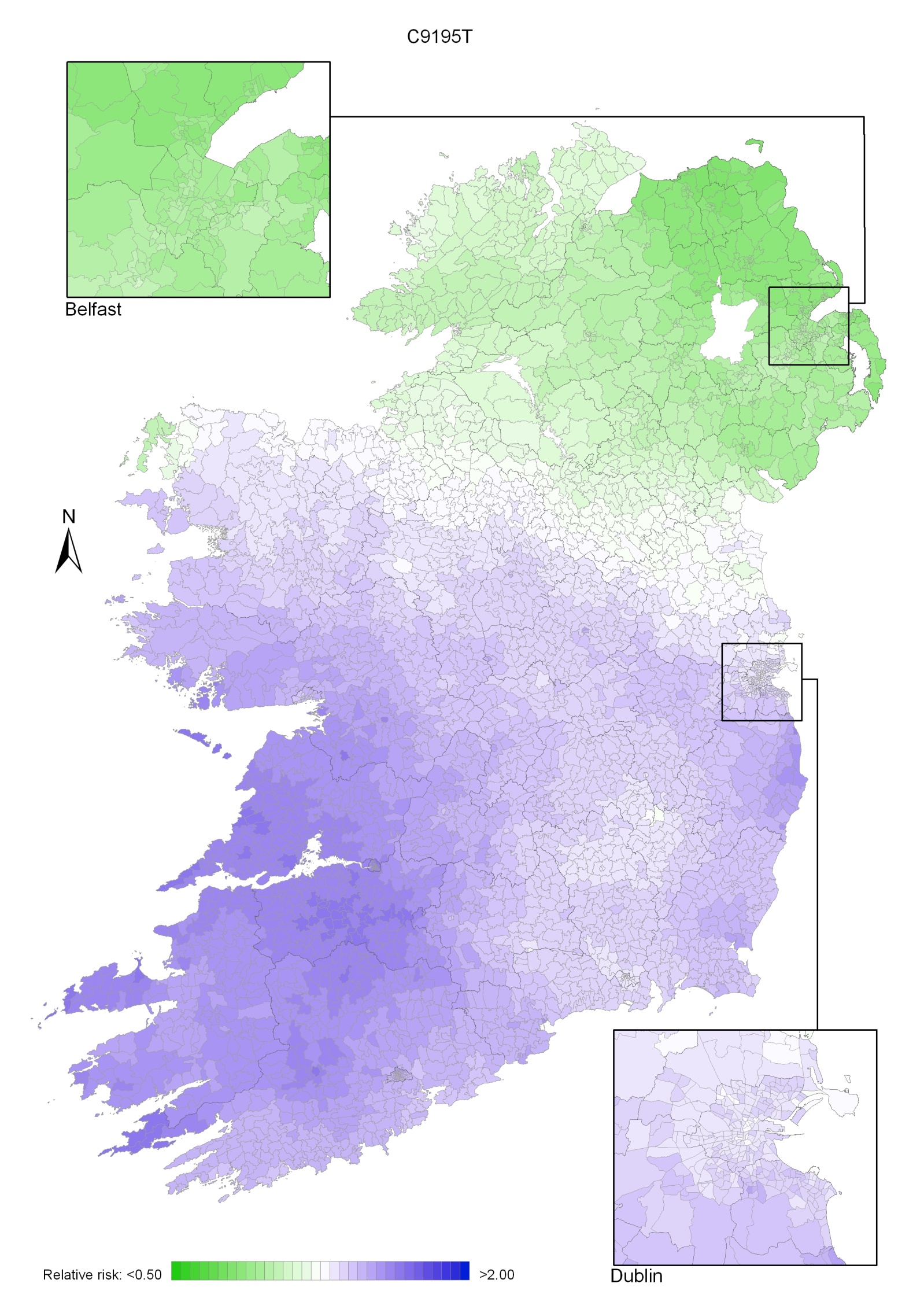
Map 13.2 Leukaemia, smoothed relative risks: males
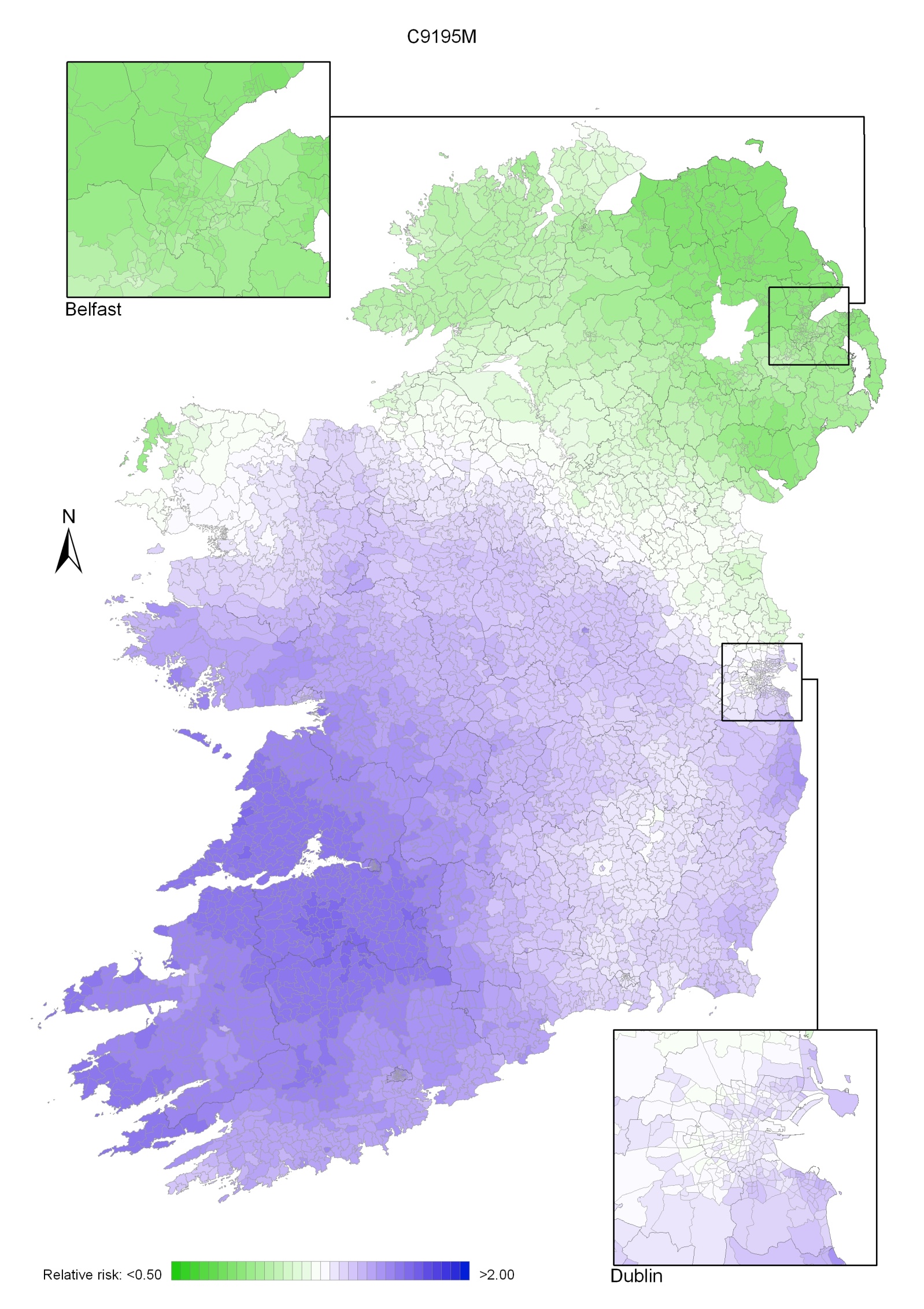
Map 13.3 Leukaemia, smoothed relative risks: females