15. Kidney cancer
15.1 Summary
Kidney cancer was the twelfth most common cancer in Ireland, accounting for 1.8% of all malignant neoplasms, excluding non-melanoma skin cancer, in women and 2.8% in men (Table 15.1). The average number of new cases diagnosed each year was 188 in women and 310 in men. During 1995-2007, the number of new cases diagnosed showed an overall increase of approximately 6% per annum in RoI; the rate of increase was lower in NI at approximately 3%.
The risk of developing kidney cancer up to the age of 74 was 1 in 188 for women and 1 in 98 for men and was similar in NI and RoI. At the end of 2008, 606 women and 959 men aged under 65, and 765 women and 1,070 men aged 65 and over, were alive up to 15 years after their kidney cancer diagnosis.
Table 15.1 Summary information for kidney cancer in Ireland, 1995-2007
Ireland | RoI | NI | ||||
female | male | female | male | female | male | |
% of all new cancer cases | 1.3% | 2.0% | 1.3% | 2.0% | 1.4% | 2.1% |
% of all new cancer cases excluding non-melanoma skin cancer | 1.8% | 2.8% | 1.8% | 2.8% | 1.9% | 2.9% |
average number of new cases per year | 188 | 310 | 123 | 214 | 65 | 96 |
cumulative risk to age 74 | 0.5% | 1.0% | 0.5% | 1.0% | 0.5% | 1.0% |
15-year prevalence (1994-2008) | 1371 | 2029 | 913 | 1407 | 458 | 622 |
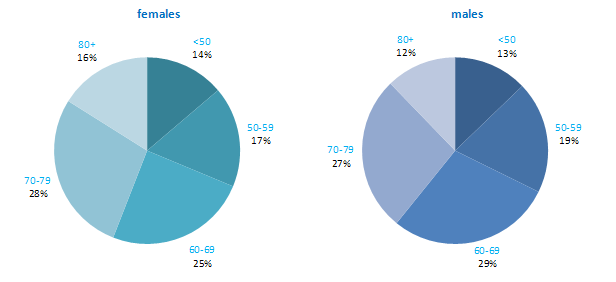
Kidney cancer is a disease of older ages, with only about 30% of new cases diagnosed in persons under 60 years old, and the majority of new cases presenting between 60 and 79 years. A significant percentage of women (16%) were diagnosed at 80 years and over (Figure 15.1). Age at diagnosis was slightly younger in RoI than in NI.
Figure 15.1 Age distribution of kidney cancer cases in Ireland, 1995-2007, by sex
15.2 International variations in incidence
Kidney cancer rates were highest in the Czech Republic, followed by the USA, for both men and women (Figure 15.2). The lowest rates occurred in Japan and Portugal for both men and women. Compared to other developed countries, the rates of kidney cancer were slightly below the median in both RoI and NI.
Figure 15.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: kidney cancer | |
| females | males |
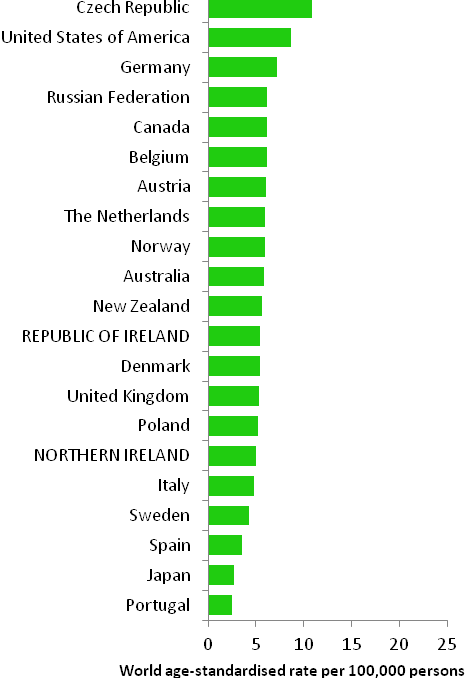 | 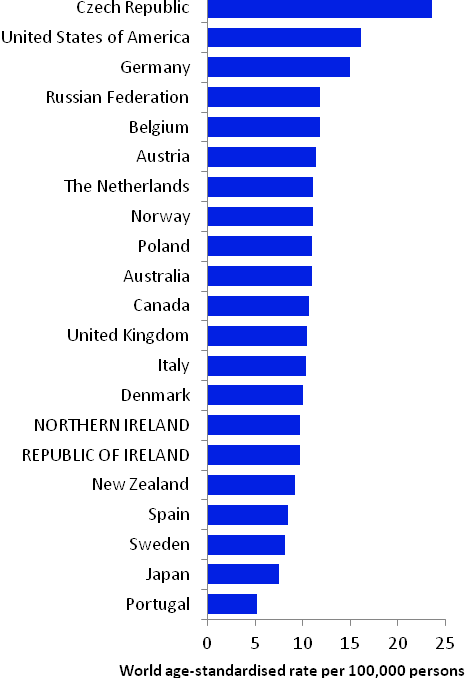 |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from Cancer Registry data for 2005-2007) NOTE: KIdney cancer was defined in GLOBOCAN 2008 by ICD10 codes C64-C66 but in this atlas we have used codes C64-C65 (see Table 2.1.). The incidence rates shown for NI and RoI in Figure 15.2 use the GLOBOCAN definition, and are consequently slightly inconsistent with data in the rest of this chapter. | |
15.3 Risk factors
Table 15.2 Risk factors for kidney cancer, by direction of association and strength of evidence
Increases risk | Decreases risk | |
Convincing or probable | Tobacco smoking1 | |
| Body fatness2,3,4 | |
| Dialysis5 | |
| High blood pressure6 | |
| Arsenic and inorganic arsenic compounds7 | |
| Cadmium and cadmium compounds7 | |
| Ionizing radiation8 | |
| Family history of kidney cancer9,10,11 | |
Possible | Smokeless tobacco12,13 | Alcohol17 |
Antihypertensive drugs6,14, 15 | ||
Occupational exposure to trichloroethylene16 | ||
1 Secretan et al., 2009; 2 World Cancer Research Fund / American Institute of Cancer Research, 2007; 3 Ildaphonse et al., 2009; 4 Mathew et al., 2009; 5 Ljunberg et al., 2011; 6 Corrao et al., 2007; 7 Straif et al., 2009; 8 El Ghissassi et al., 2009; 9 one or more first degree relative(s) with cancer of the kidney; 10 Hung et al., 2007; 11 Clague et al., 2009; 12 chewing tobacco or snuff; 13 Lee and Hamling, 2009; 14 diuretic and non-diuretic; 15 Grossman et al., 2001; 16 Kelsh et al., 2010; 17 Lee et al., 2007 | ||
The two most common types of kidney cancer are renal cell carcinoma and urothelial cell carcinoma of the renal pelvis; the majority (over 90%) are renal cell carcinomas. Tobacco smoking is causally associated with renal cell cancer in both men and women (Table 15.2): there is a dose-response relationship with number of cigarettes smoked and, in some studies, risk reduces after cessation of smoking (International Agency for Research on Cancer, 2004b). An association between use of smokeless tobacco and kidney cancers in general has also been suggested.
As regards other lifestyle-related risk factors, pooled analysis of prospective studies suggests that drinking alcohol may be associated with a moderately decreased risk of renal cell cancers. In contrast, studies consistently show that body fatness is associated with elevated risk. Overall, risk increases by almost one-third per 5kg/m2 increase in body mass index and perhaps to a slightly greater extent in women than men.
Advanced kidney disease, which makes dialysis necessary, raises the risk of renal cell cancer, but the underlying mechanism is unclear. Hypertension has also been associated with a 60% increased risk of renal cell cancer. Risk may also be raised in those who have used antihypertensive drugs, but whether the associations hold in men and women and after adjustment for other risk factors is somewhat uncertain.
Exposure to cadmium and cadmium compounds, which generally takes place occupationally, and to arsenic or inorganic arsenic compounds, which may be occupational or ingested in food or drinking water, is likely to cause kidney cancer. Occupational exposure to tricholoroethylene, a hydrocarbon commonly used as an industrial solvent, has been associated with a modestly raised risk, but concerns remain about whether the association could be due to uncontrolled confounding.
After accounting for other risk factors, risk of kidney cancer in general, and renal cell cancer in particular, is increased by between 40% and 100% in those with at least one affected first degree relative.
15.4 Small geographic area characteristics and cancer risk
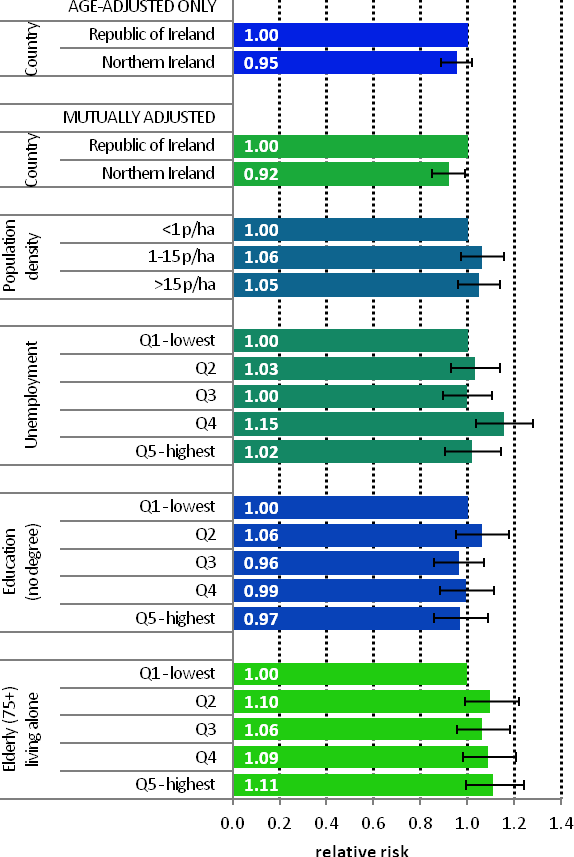
Figure 15.3 Adjusted relative risks (with 95% confidence intervals) of kidney cancer by socio-economic characteristics of geographic area of residence: males | MalesAdjusting for age alone, there was no significant difference between RoI and NI in the risk of kidney cancer in men during 1995-2007 (Figure 15.3). However once adjustments for population density and socio-economic factors were made, a lower relative risk for NI, compared to RoI, of 0.92 (95%CI=0.85-0.99) was identified. There was no association between male kidney cancer risk and population density, educational attainment or socio-economic characteristics, although quintile 4 of the unemployment area-based measure had a slightly elevated rate of kidney cancer. |
Figure 15.4 Adjusted relative risks (with 95% confidence intervals) of kidney cancer by socio-economic characteristics of geographic area of residence: females
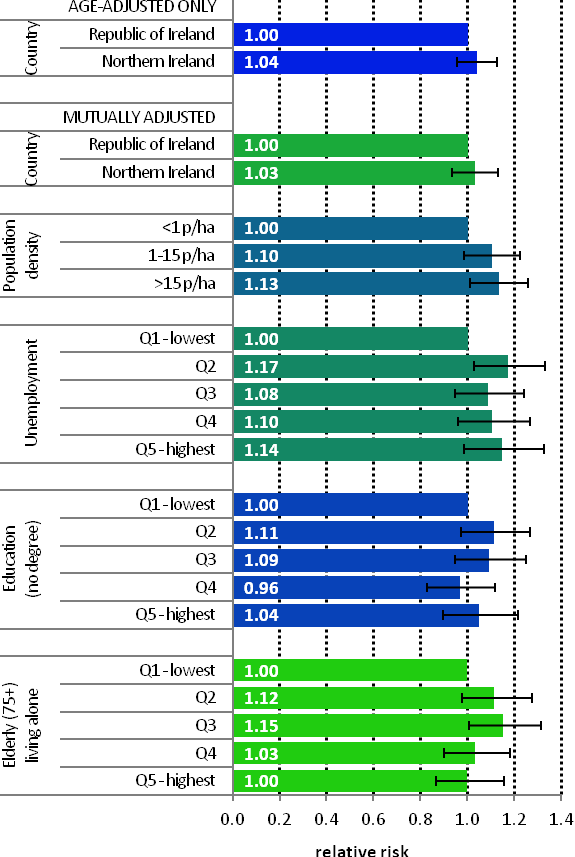
| FemalesThe risk of kidney cancer in women did not differ significantly between RoI and NI (Figure 15.4). There was a weak positive association between female kidney cancer and population density, with those resident in the most densely populated areas having a 13% greater risk than those in the least dense areas. There were no overall associations with socio-economic characteristics and kidney cancer among women, although those resident in quintile 2 of the unemployment measure, and quintile 3 of the elderly living alone measure had an elevated risk of the disease. |
15.5 Mapping and geographical variation
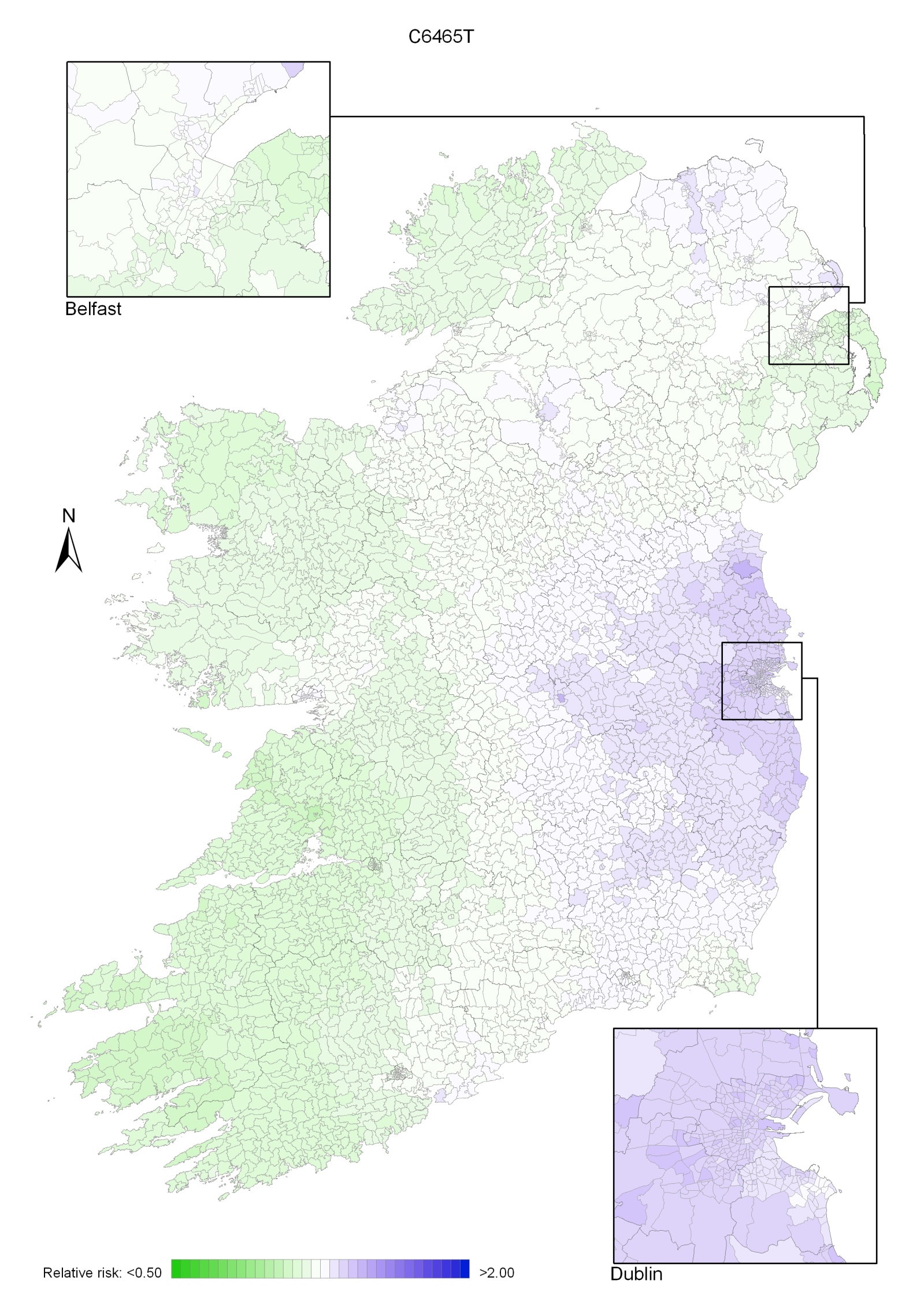
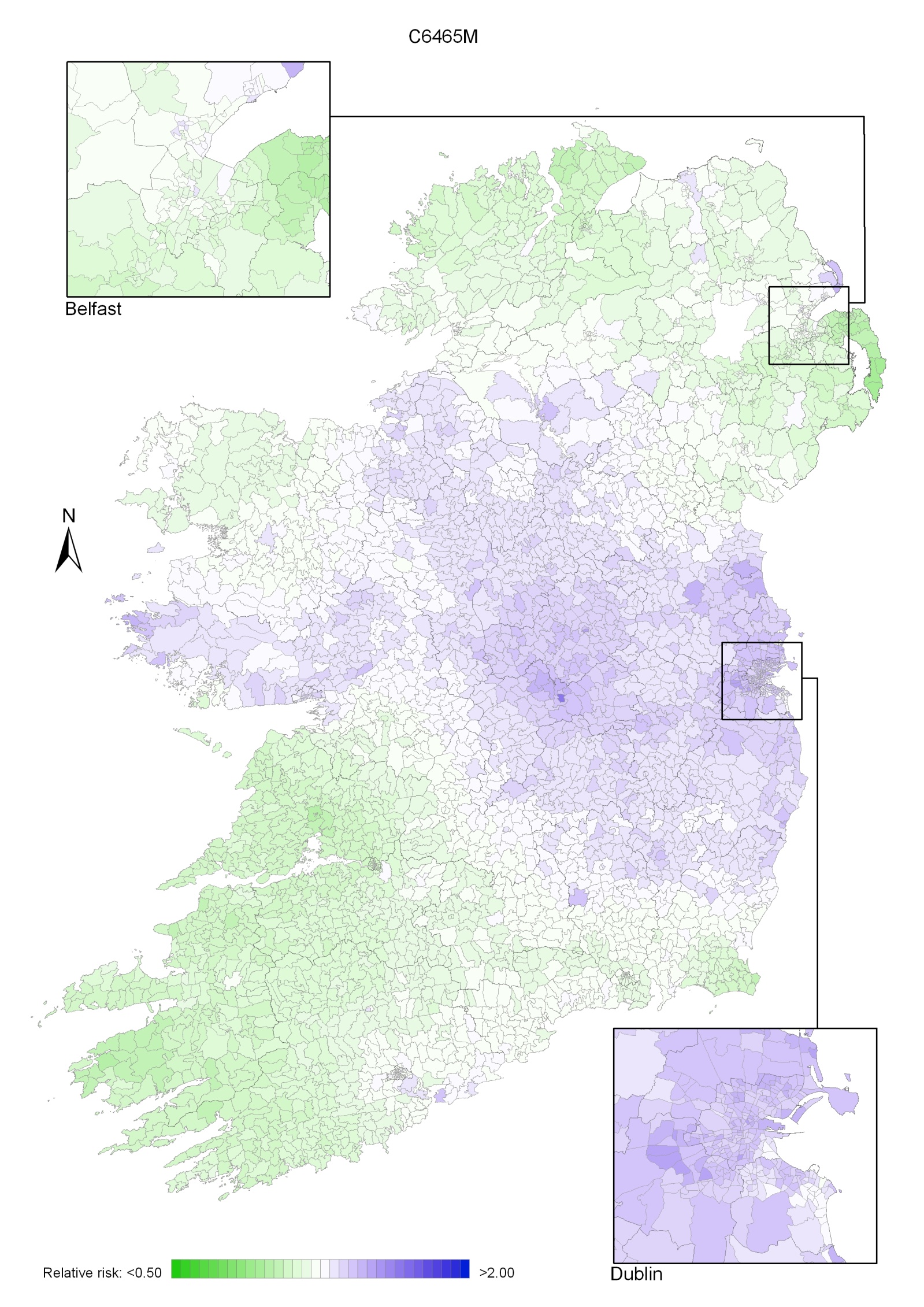
The geographical pattern of relative risk for kidney cancer showed only modest variation, which was different for men and women (Maps 15.1-15.3).
For both sexes combined, the area of highest relative risk was mainly confined to Leinster, with lower relative risks in the western half of Ireland (Map 15.1).
For men, the relative risk was higher in a wide band across the country extending from Sligo to Wexford. The relative risks were lower in the south-west and north (Map 15.2).
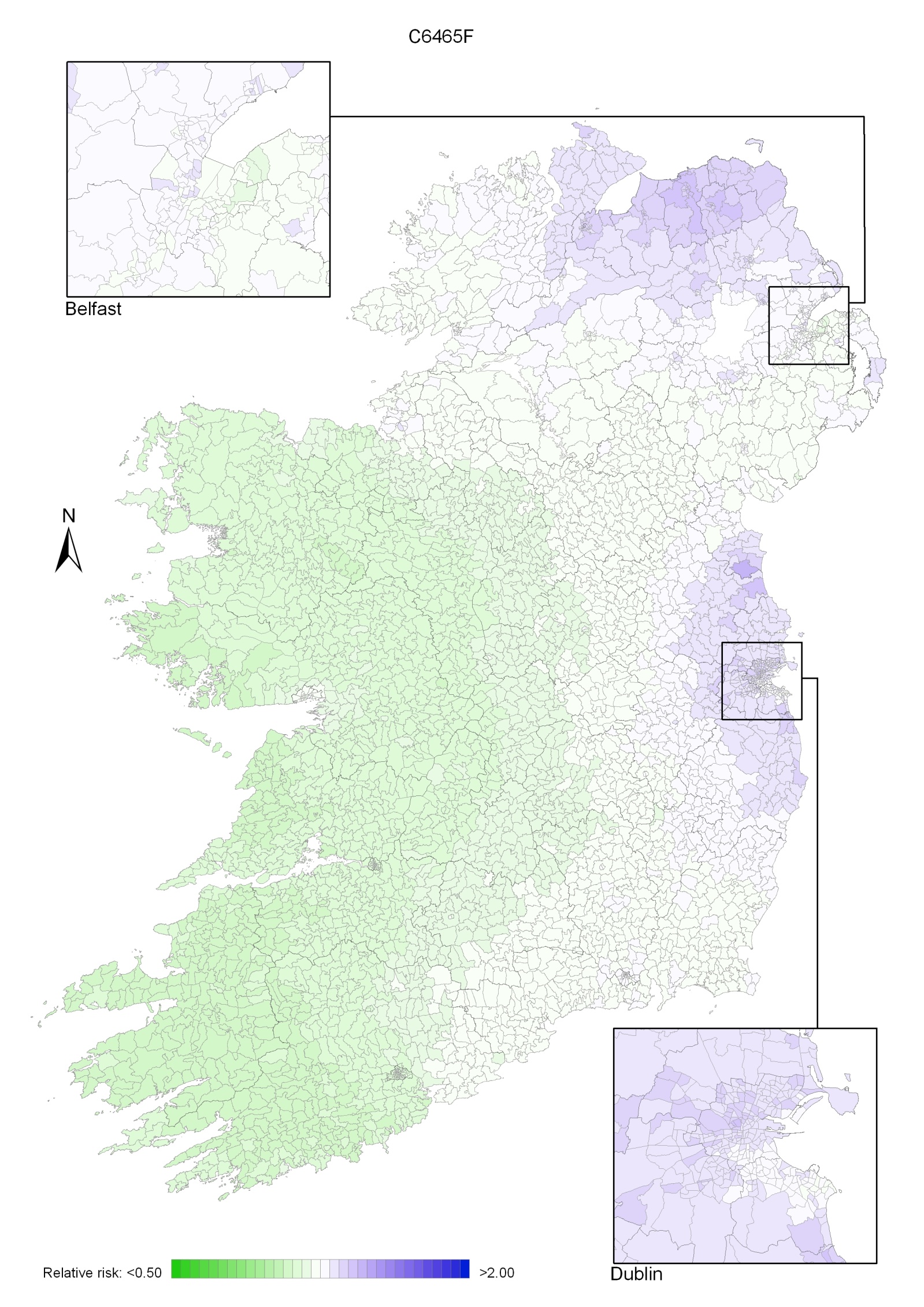
For women, there were just two areas of higher relative risk, along the north coast (from Donegal in RoI to Moyle/Larne in NI) and in the area from Louth to Wicklow, while the west had lower relative risks (Map 15.3).
Map 15.1 Kidney cancer, smoothed relative risks: both sexes
Map 15.2 Kidney cancer, smoothed relative risks: males
Map 15.3 Kidney cancer, smoothed relative risks: females