17. Ovarian cancer
17.1 Summary
Ovarian cancer was the fourth most common cancer for women in Ireland, accounting for 4.6% of all malignant neoplasms, excluding non-melanoma skin cancer (Table 17.1). The average number of new cases diagnosed each year was 479. During 1995-2007, there was little change in the number of new cases diagnosed per year in RoI while the numbers decreased slightly in NI.
The risk of developing ovarian cancer up to the age of 74 was 1 in 71 and was similar in NI and RoI. At the end of 2008, 1,441 women aged under 65 and 994 women aged 65 and over were alive up to 15 years after their cancer diagnosis.
Table 17.1 Summary information for ovarian cancer in Ireland, 1995-2007
Ireland | RoI | NI | |
% of all new cancer cases | 3.4% | 3.3% | 3.5% |
% of all new cancer cases excluding non-melanoma skin cancer | 4.6% | 4.6% | 4.6% |
average number of new cases per year | 479 | 319 | 159 |
cumulative risk to age 74 | 1.4% | 1.4% | 1.4% |
15-year prevalence (1994-2008) | 2435 | 1564 | 871 |
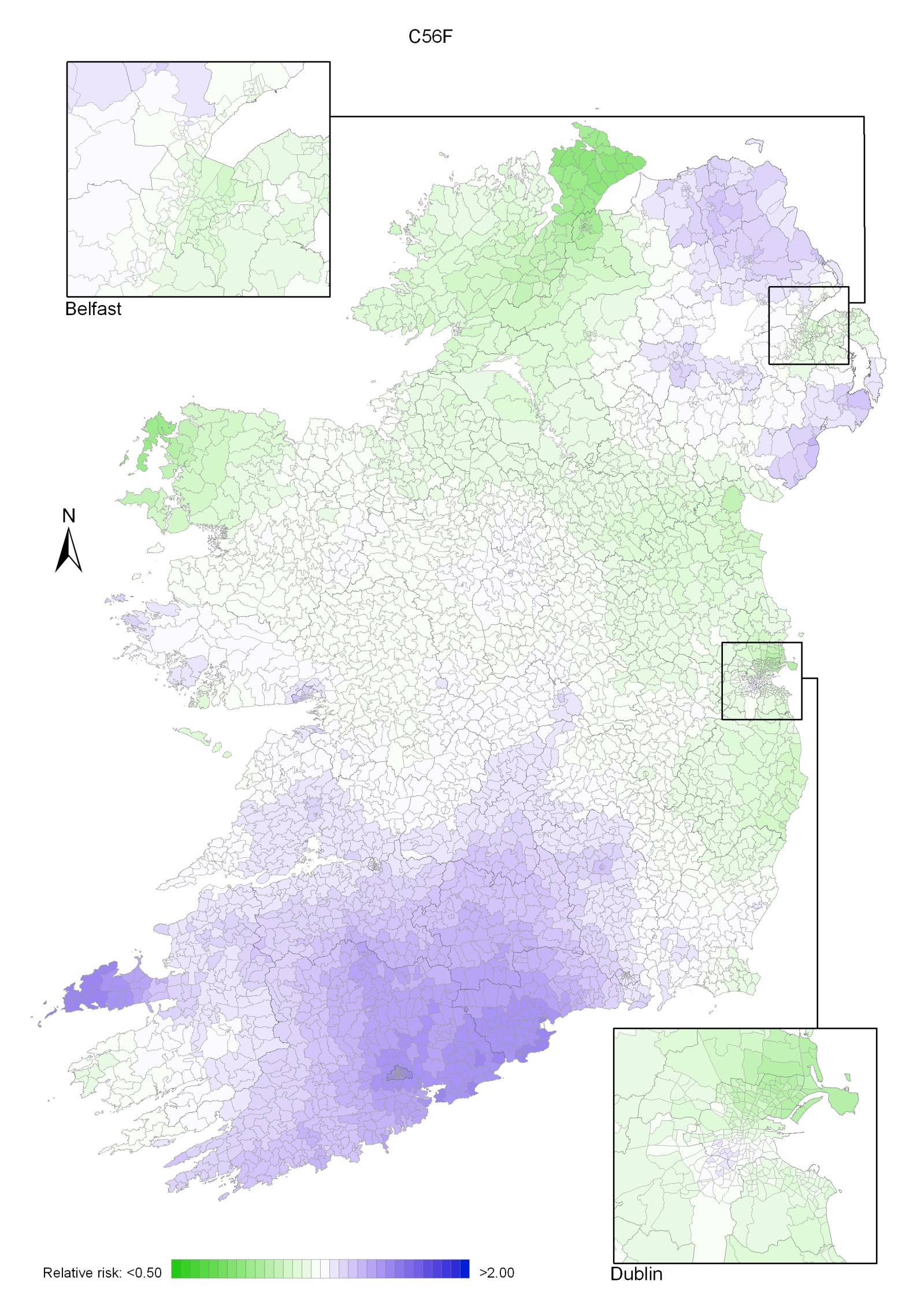
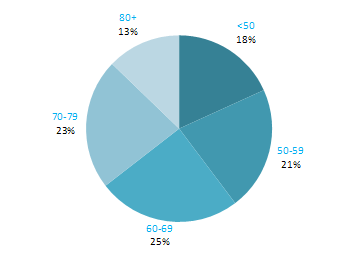
The age distribution of ovarian cancer at diagnosis was more uniform than for most other cancers (Figure 17.1). Approximately 18% of cases presented under 50 years of age, 21% between 50 and 59, 25% between 60 and 69 and 23% between 70 and 79; the remainder (13%) presented at 80 years or over. There was a similar age pattern in RoI and NI.
Figure 17.1 Age distribution of ovarian cancer cases in Ireland, 1995-2007
17.2 International variations in incidence
In 2008, estimated rates of ovarian cancer were high in the UK, RoI and NI and also in Poland and the Czech Republic (Figure 17.2). Rates of the disease were lowest in Portugal, followed by Japan, Australia and Canada. Differences in the coding of borderline ovarian cancers by cancer registries may account for some of the international differences in incidence rate.
Figure 17.2 Estimated incidence rate per 100,000 in 2008 for selected developed countries compared to 2005-2007 incidence rate for RoI and NI: ovarian cancer |
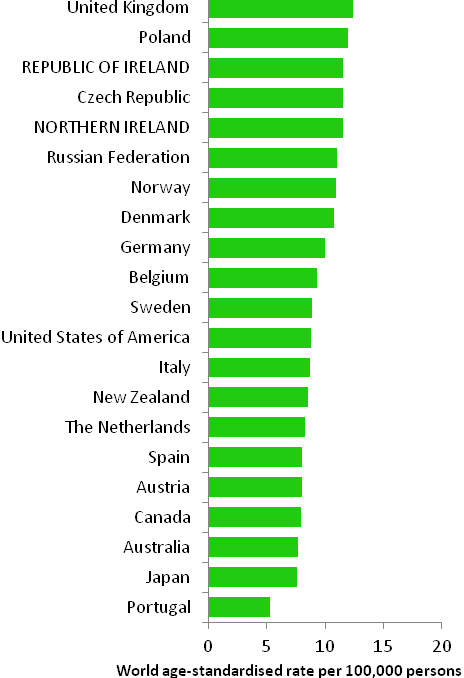 |
Source: GLOBOCAN 2008 (Ferlay et al., 2008) (excluding RoI and NI data, which is derived from Cancer Registry data for 2005-2007) |
17.3 Risk factors
Table 17.2 Risk factors for ovarian cancer, by direction of association and strength of evidence
| Increases risk | Decreases risk |
Convincing or probable | Family history of ovarian cancer1,2 | Tubal ligation13 or hysterectomy with ovarian conservation11,14 |
| Nulliparity3 | Oral contraceptives6,15,16,17 |
| Hormone replacement therapy4,5,6 | |
| Height/tallness7 | |
| Tobacco smoking8,9 | |
| Asbestos10 | |
Possible | Fertility drugs3,11 | Breast feeding18 |
Greater body fatness7,12 | Non-starchy vegetables19,20 | |
Physical activity21 | ||
1 one or more first degree relative(s) with cancer of the ovary; 2 Stratton et al., 1998; 3 Ness et al., 2002; 4 particularly oestrogen-only formulations; 5 Pearce et al., 2009; 6 International Agency for Research on Cancer, 2011a; 7 Schouten et al., 2008; 8 associated with mucinous tumours only; 9 Secretan et al., 2009; 10 Straif et al., 2009; 11 Whittemore et al., 1992; 12 Lahmann et al., 2010; 13 surgical procedure involving cutting or blocking a woman’s fallopian tubes; 14 Cibula et al., 2011; 15 combined oestrogen-progestogen formulations; 16 Collaborative Group, 2008; 17 Cibula et al., 2010; 18 Ip et al., 2009; 19 includes broccoli, cabbage, carrots, cauliflower, celery, leeks, lettuce, onions, peas, peppers and spinach; 20 World Cancer Research Fund / American Institute of Cancer Research, 2007; 21 Olsen et al., 2007 | ||
Family history of the disease is the most important risk factor for ovarian cancer. Women with at least one affected first degree relative have a three-fold increased risk of developing ovarian cancer themselves. Together with breast cancer, ovarian cancer is a component of several autosomal dominant cancer syndromes, most notably the BRCA1 and BRCA2 mutation syndromes. Women who have mutations in the BRCA1 or BRCA2 genes have a high chance of developing ovarian cancer over their lifetime (39% risk for BRCA1 mutation carriers and 11% for BRCA2 mutation carriers up to the age of 70; Antoniou et al., 2003).
Endogenous and exogenous oestrogens play a key role in the aetiology of ovarian cancer. Not having children (nulliparity) is associated with increased risk and, by contrast, each additional child confers a 20% reduction in risk (Riman et al., 2004). Women who have used fertility drugs may also have raised risk, especially if they remain nulligravid. Risk is reduced in women who have had bilateral tubal ligation (their fallopian tubes “tied”) or hysterectomy with ovarian conservation. In terms of exogenous hormones, use of hormone replacement therapy, particularly oestrogen-only formulations, is clearly related to increased risk, although formulations which include progestin are associated with only a modest risk. Women who have used combined oestrogen-progestogen oral contraceptives have decreased risk. Protection increases with increasing duration of use, and the reduction in risk persists for more than 30 years after use has ceased. Breastfeeding has also been associated with lower risk of ovarian cancer, but uncertainties remain in the evidence.
Risk of ovarian cancer is raised in taller women, but tallness in itself is unlikely to be a causal factor; it is most likely a marker for factors relating to promoters of growth in childhood (World Cancer Research Fund / American Institute of Cancer Research, 2007).
Several lifestyle factors have been related to ovarian cancer risk, but most of the associations remain somewhat uncertain. The exception is smoking, which is causally related to mucinous ovarian tumours, but not to other tumour types (Jordan et al., 2006). Higher intake of non-starchy vegetables may be associated with reduced risk, but this category includes a wide and disparate group of vegetables with many different plant food constituents (e.g. fibre, folate, flavonoids) and the contributions of the different constituents have not been unravelled (World Cancer Research Fund / American Institute of Cancer Research, 2007). There may be a modest (approximately 20%) reduction in risk among women with the highest, versus those with the lowest, levels of recreational physical activity. Body fatness and/or obesity may also be related to increased risk.
17.4 Small geographic area characteristics and cancer risk
Figure 17.3 Adjusted relative risks (with 95% confidence intervals) of ovarian cancer by socio-economic characteristics of geographic area of residence | |
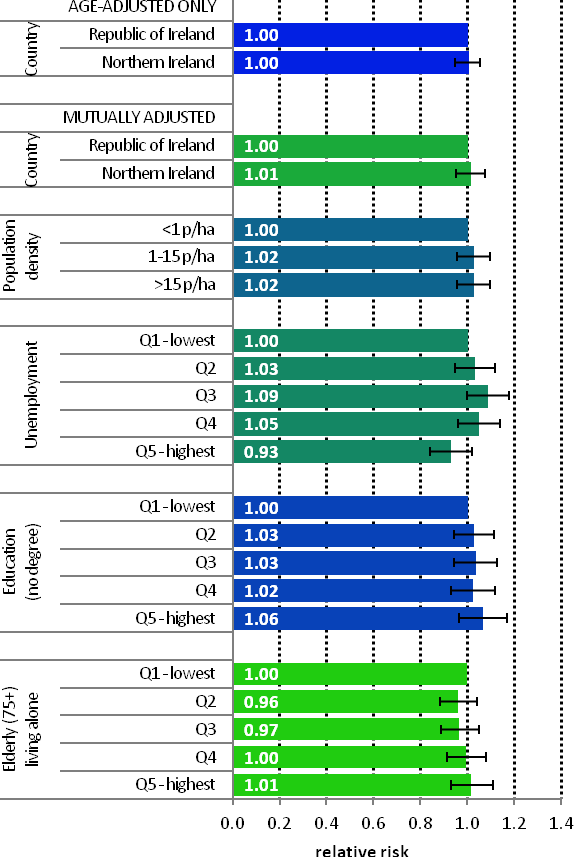 | The risk of ovarian cancer was similar in NI and RoI during 1995-2007, both with and without adjustment for socio-economic and population density factors (Figure 17.3). Variation in ovarian cancer risk by area-based socio-economic characteristics and population density was minimal. However, women living in areas with unemployment of between 4.8% and 6.2% (quintile 3) had a 9% elevated risk of this cancer. |
17.5 Mapping and geographical variation
Ovarian cancer showed a strong geographical pattern with two main areas of higher relative risk (Map 17.1). The first area was centred on Cork city, extending over most of Munster and including the Dingle peninsula in particular. The second area was in the eastern half of NI.
Map 17.1 Ovarian cancer, smoothed relative risks