

This atlas demonstrates, for the island of Ireland, many of the patterns already seen in the cancer atlas of the Republic of Ireland (Carsin et al. 2009), but the inclusion of Northern Ireland allows some geographical trends to be seen more clearly. The juxtaposition of two similar populations with different health services is also of interest. Recorded variation in cancer rates across geographical areas may be attributed to three factors—true geographical variation in the underlying risk of cancer, differences in case ascertainment and definition, and random variation. The hypothesis suggested in this atlas is that the geographical variation is largely due to variation in cancer risk.
The mapping presented in this atlas shows a wide diversity of geographical patterns of risk, many of which are difficult to interpret. Mapping demonstrated broadly similar geographical patterns for men and women for most cancers. Three cancers (pancreas, brain and other central nervous system, and leukaemia) had an increasing gradient of risk from north-east to south-west, but apart from this there was no consistent gradient of risk across the island. There was a marked geographical variation in the risk of some common cancers—melanoma and non-melanoma skin, lung, prostate, oesophagus, stomach and gynaecological cancers—but very little for others—breast, colorectal and non-Hodgkin’s lymphoma.
Overall, the relationships between socio-economic variables and cancer risk were similar for men and women. The strength of the relationship, and consequently the statistical significance, varied, but we did not observe any situation in which the effects of socio-economic factors were in opposite directions for men and women. Patterns consistent with known socio-economic gradients in cancer risk (Faggiano et al., 1997) were observed. Cancers of lung, stomach and head and neck in both sexes, colorectal, bladder and pancreas cancer in men and cervical cancer in women were all more common in areas of higher unemployment. Areas where a smaller proportion of the population had third-level qualifications had a higher risk of lung cancer (particularly in women) and stomach cancer in both sexes, and of cervical cancer and pancreatic cancer in women. Conversely, where unemployment was lower and/or educational levels higher, prostate and female breast cancer, as well as melanoma and non-melanoma skin cancer, were more common.
Most cancers were more frequent in urban areas (as measured by population density), after adjusting for the effect of age. This relationship was statistically significant for non-melanoma skin, colorectal, lung, stomach, bladder, head and neck and oesophageal cancer in both sexes and for breast, cervical, kidney and brain and other CNS cancer in women; a reciprocal relationship was seen only for prostate cancer.
We have previously noted a consistent, if weak, relationship between cancer and the percentage of people aged 65 and older living alone in RoI (Carsin et al., 2009). For this report, the cut-off point was set at 75 years and older, for compatibility between census measures in the two countries, and the relationship was not as consistently observed. However, a positive relationship was observed between increased cancer risk and an increased percentage of persons aged 75 and older living alone for non-melanoma skin, lung, breast, colorectal, stomach, pancreas, bladder, head and neck and oesophageal cancer and for leukaemia, for one or both sexes. This relationship was independent of the measures of deprivation used here, but may be a marker of area-based types of “deprivation”, such as poor diet and chronic ill-health, not identified by the conventional indices (Harrington et al., 2011; Layte et al., 2011). However, it may also be a marker of individual risk. In RoI in 2006, 46% of the population aged 75 and older was widowed and 19% unmarried, so most of those aged 75 and older and living alone are also likely to have been widowed (Central Statistics Office, 2007). Premature bereavement may be an indicator of a shared higher risk lifestyle.
The relative risk of developing many of the cancers presented here was higher in RoI than in NI. The risk of non-melanoma skin cancer, melanoma, leukaemia, bladder, pancreas and brain/central nervous system cancer was significantly higher for both sexes in RoI. For men, the risk of prostate cancer was higher in RoI and, for women, cancer of the oesophagus and cervix. In NI, the risk of lung cancer was higher for both sexes as was that of non-Hodgkin’s lymphoma, head and neck cancers and cancer of the corpus uteri for women.
The possibility therefore exists that some of these differences are due to the methods by which cases are registered. The completeness of registration is very high in both registries and differences in case ascertainment are unlikely to contribute substantially to the differences in cancer risk found. The two registries identify and code cancer cases in very similar ways and adhere to the agreed international guidelines on quality assurance in registration. However, the demarcation between frankly malignant, borderline malignant and benign cancers is not always clear. Slight variations in how these cancers are reported by histopathologists, and how these reports are interpreted by registries, may lead to systematic differences in reported incidence rates. In the course of a number of collaborative projects by the two Irish registries (Donnelly et al., 2009, Campo et al., 2004, Walsh et al., 2001) we have identified the situations in which such discrepancies might occur (e.g. for bladder and ovarian cancer) and we are satisfied that there are no significant differences between the registries in registration practices.
The element of random variation is important in interpreting geographical variation in cancer risk. By using as long a time period as possible to maximise the number of cases in each small area, and well-developed smoothing methods, we have considerably reduced the contribution of random variation. However, for areas which have very small populations, or are geographically isolated, and for some of the less common cancers, smoothing is less effective and it is likely that some of the small variations in risk shown on the maps are due to random variation in incidence, unrelated to underlying risk.
The aetiology of most cancers is a complex interplay between environmental (in the broadest sense) and genetic factors. Genetic factors might be responsible for a little of the geographical variation seen, but genetic variation is an improbable overall explanation for the patterns reported here. There is little evidence for significant heterogeneity (O’Dushlaine et al., 2008) or geographical variation (Hill et al., 2000, Dolan et al., 2005) in the genetic makeup of the Irish population, although Dolan et al (2005) report a small north-east/south-west gradient in polymorphisms of some pathogen-response-associated genes.
Differing levels of cancer detection, case-finding or screening may result in higher disease rates in one area compared with another. For example, asymptomatic prostate cancer cases will be picked up sooner and probably at a higher rate if an area has a higher level of prostate-specific antigen testing. This will result in an apparently higher risk of prostate cancer in the target population. Chronic lymphocytic leukaemia (CLL), a disease of older persons which is usually only identified by a blood test and is frequently asymptomatic, will often be detected only if the person happens to have a blood count. Increased use of CT scans of the abdomen for other illnesses will increase the detection of occult intra-abdominal cancer e.g. kidney cancer. Organised screening, for instance for breast and cervical cancer, will result in an increase in incidence at the beginning of the screening programme, and possibly for longer.
The contribution of lifestyle factors to variation in cancer risk is well known. Tobacco use is the best-established of these; it has a clear geographical pattern of prevalence in Ireland and causes the largest increase in relative risk. In addition, diet, exercise, obesity, sun exposure and alcohol use are known risk factors, the prevalence of which is also known to vary with area of residence. Since we lack detailed information on the spatial distribution of these risk factors in Ireland, in this report we have used area-based measures such as population density, unemployment and level of educational attainment as partial proxies for lifestyle. Where data (however limited) on geographical variation in known risk factors was available we present it below.
Smoking is clearly established as a cause of many cancers (Secretan et al., 2009). The highest smoking prevalence in NI in 2010 (26% for men and 28% for women) was in the Western Health and Social Services Board¶ (HSSB) (Northern Ireland Statistics and Research Agency, 2010b) (Figure 21.1). The lowest smoking prevalence for men (22%) was in the Northern HSSB and for women (19%) in the Southern HSSB.
In RoI in 1998 smoking prevalence was 32% for men and 31% for women. By 2003 these had fallen to 30% and 27% respectively (Office of Tobacco Control, 2010). In RoI, there was a clear geographical pattern in 2003, with overall prevalence in Dublin at 32%, in the rest of Leinster¶ 29%, in Munster 27% and in Connacht 25%. However by 2010, smoking prevalence was highest in the RoI Health Service Executive (HSE) South region¶ (which covers much of Munster) (Figure 21.1) (Office of Tobacco Control, 2010).
| Figure 21.1 Smoking prevalence in Health and Social Services Boards and HSE regions, 2009-2010 |
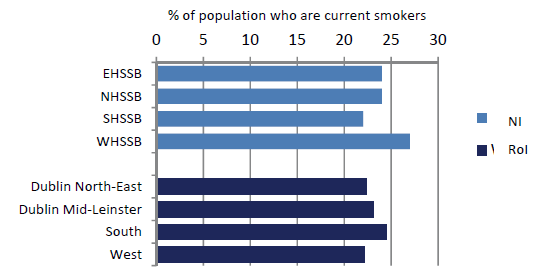 |
Figures refer to the population aged 15 years and over in RoI and 16 years and over in NI. |
While smoking prevalence in 2003 can have no direct bearing on cancer risk in 1995-2007, due to the lag time for development of cancer, these geographical patterns are likely to reflect long-term differentials. Looking at the tobacco-related cancers, the geographical distribution of lung cancer clearly reflects the higher cigarette consumption in the east of RoI, as does that for cervical cancer. Cancers of oesophagus and bladder also have an east-west gradient, but this is less marked, consistent with their more complex aetiology.
Alcohol has been established as a causative factor in breast, colorectal, head and neck, pancreatic and oesophageal cancers (Secretan et al., 2009). In NI, the percentage of drinkers exceeding the “sensible” weekly limits in 2008 was highest in the Eastern HSSB (28%), and lowest in the Southern HSSB (20%) (Department of Health, Social Services and Public Safety, 2008). There was some geographical variation in the prevalence of alcohol consumption in 2007 in RoI (Morgan et al., 2009). The highest prevalence was in Dublin, with 84-85% regular drinkers, followed by Cork and Kerry (76%), with a fairly even prevalence in the rest of the country of 73-74%.
Alcohol-related cancers had a variety of geographical patterns. Colorectal cancer was commonest in the south, and in the east around Dublin and in much of NI for women, breast cancer was most common in the east, pancreatic cancer in the south-west and oesophageal cancer in the east and south. There was no overall geographical pattern for head and neck cancers. The pattern of oesophageal cancer risk was closest to that of higher alcohol consumption, but, as with tobacco, it cannot be assumed that current consumption patterns reflect of those two decades ago.
Obesity has been shown to be a risk factor for breast, colorectal, pancreas, kidney, oesophagus, and corpus uteri cancers, and may be a risk factor for NHL, melanoma, leukaemia and cancers of prostate and ovary (World Cancer Research Fund/American Institute for Cancer Research, 2007).
In 2005-2006 levels of obesity (measured, not self-reported) were higher overall in RoI than in NI (Figure 21.2) and, within RoI, in the west and south-west (Morgan et al., 2009). In NI the prevalence of obesity was highest in the Southern HSSB (Northern Ireland Statistics and Research Agency, 2010b). The lowest levels of obesity were in urban areas—Dublin in RoI and the Eastern HSSB (which includes Belfast) in NI, and in the Mid-West region in RoI.
| Figure 21.2 Percentage of Irish population who were overweight or obese, by area of residence, 2005-2006 |
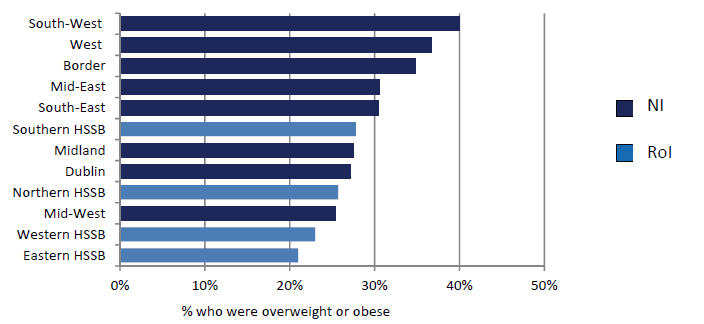 |
Note: The regions shown for NI are Health and Social Services boards and for RoI the NUTS level 3 regions (see Appendix table A4.1). |
The two main infective causes of cancer in the Irish population are Helicobacter pylori, which causes stomach cancer and human papilloma virus (HPV), which causes cervical cancer, some head and neck cancers and non-melanoma skin cancers.
The reported prevalence of H pylori in a random sample of 1000 blood donors in RoI in 1998 was reported as 43%, and 62% in those aged 46-60 (Buckley et al., 1998). 504 individuals aged 35 to 74 sampled in Cork and Kerry in 1997/1998 had a prevalence of 61% (Sheehan et al., 2005a) and in a sample from a population study of cardiovascular risk in NI in 1986/1987 the prevalence was 50% overall and 67% in those aged 45-59 (Murray et al., 1997). A survey of 104 Irish university students (Sheehan et al., 2004b) yielded a prevalence of 59%, a very high value for a young cohort. The NI samples showed a clear social class gradient, with a prevalence of 43% in social class I and 68% in social class V. Inadequate sanitation and crowded housing appear to be related to higher rates of H pylori infection (Brown, 2000).
HPV prevalence in a sample of women presenting for cervical screening in the Dublin area of RoI in 2004-2005 was reported as 19.8% (Keegan et al., 2007). No information has been published on geographical variation in infection rates in RoI. The crude prevalence of high risk HPV for women in the NI Screening programme was reported to be 18.1% in 2008 (personal communication)
For other important aetiological factors—including UV exposure, patterns of child-bearing and use of medications such as hormone replacement therapy, oral contraceptives and non-steroidal anti-inflammatory drugs—little information is available on geographical or socio-economic variation in prevalence, and most of what exists (Boyle et al., 2010; Corcoran et al., 1996) pertains to recent periods. Information on occupational and environmental exposures is equally scanty.
A number of surveys of diet, lifestyle and physical activity have been published in RoI (Friel et al., 1999; Kelleher et al., 2003; Harrington et al., 2008; Morgan et al., 2008; Morgan et al., 2009) but contain very little information on geographical variation in risk factor prevalence other than for the largest geographical units.
¶ Information on Health and Social Services boards, provinces, health service regions, and their constituent counties and district councils, is given in Appendix table A4.1.
The risk of non-melanoma skin cancer (NMSC) was highest in two types of area—in and around the major urban centres in RoI (but not around Belfast and Derry in NI) and in a number of coastal areas in both RoI and NI. The aetiology of this cancer is better understood than that of most other cancers. Apart from some uncommon exposures—immunosuppressants, arsenic—NMSC in light-skinned people is caused by UV exposure (International Agency for Research on Cancer, 1992; Armstrong and Kricker, 2001). A survey of urban dwellers in RoI in 1991 showed that the great majority were light-skinned and at high risk of skin cancer from UV exposure (Gibson et al., 1997). No information is available on the geographical distribution of skin types within Ireland.
UV exposure may be recreational, including sunbed use (Karagas et al., 2002; Boyle et al., 2010), or occupational—the main occupations involved in the past being farming, fishing and building work. Gibson et al. (1997) found that 16% of their sample had used sunbeds. Higher recreational exposures have been reported among the more affluent in Ireland (Corcoran et al., 1996; Boyle et al., 2010). In a random sample of 2,200 people in NI, subjects with higher education attainment were more likely to report that having a suntan made them feel “healthier” or “more attractive”, and to have used sunbeds in the past. 20% of the sample had used sunbeds in 2008, down from 28% in 2000. A survey in 1993 of people taking “sun holidays” from Dublin airport, 11% of whom lived in NI, showed a predominance of professional and non-manual workers, with only 11% describing themselves as “manual workers”, compared to 31% in the general population in the 1991 census (Corcoran et al., 1996).
The distribution of men involved in farming, fishing and other agricultural work is likely to vary considerably across the island, and is a possible explanatory factor for geographical variation in NMSC risk. As NMSC development requires long UV exposure, we looked at the occupational distribution by county as given in the 1981 censuses, 20 years before the midpoint of the period covered by this report (Central Statistics Office, 1986; Northern Ireland Statistics and Research Agency, 1982). Table 21.1 shows the percentage of men reported as being involved in outdoor occupations (with the exception of the building trades, for which there was no separate category) in 1981 (Central Statistics Office, 1986; Northern Ireland Statistics and Research Agency, 1982). It is noticeable that the highest percentages in these occupations were in mostly inland counties of RoI, and the lowest in NI and there seems to be no relationship at county/district council level to the distribution of NMSC risk.
Table 21.1 Percentage of male population in Ireland employed in agriculture, forestry and fishing, 1981 | |||
county/district council | % of population aged 15 and over employed in agriculture, forestry and fishing | county/district council | % of population aged 15 and over employed in agriculture, forestry and fishing |
|---|---|---|---|
Roscommon | 34% | Omagh | 13% |
Leitrim | 34% | Wicklow | 13% |
Cavan | 33% | Kildare | 13% |
Mayo | 31% | Dungannon | 13% |
Longford | 28% | Magherafelt | 12% |
Monaghan | 27% | Armagh | 12% |
Tipperary | 26% | Strabane | 12% |
Clare | 26% | Banbridge | 12% |
Galway | 26% | Limavady | 10% |
Kerry | 25% | Newry and Mourne | 9% |
Laois | 25% | Down | 9% |
Sligo | 24% | Louth | 9% |
Kilkenny | 23% | Ballymena | 8% |
Wexford | 23% | Ards | 7% |
Donegal | 21% | Coleraine | 7% |
Meath | 21% | Antrim | 6% |
Offaly | 20% | Larne | 6% |
Carlow | 20% | Lisburn | 4% |
Westmeath | 18% | Craigavon | 4% |
Fermanagh | 16% | Derry | 3% |
Moyle | 16% | Newtonabbey | 2% |
Cork | 16% | Carrickfergus | 2% |
Limerick | 15% | Castlereagh | 2% |
Waterford | 15% | Dublin | 1% |
Cookstown | 14% | North Down | 1% |
Ballymoney | 14% | Belfast | <1% |
Ascertainment bias may account for part of the apparently higher NMSC risk in urban areas. NMSC is relatively asymptomatic and rarely fatal, which makes it likely that a significant number of cases escape medical attention. Rural populations are further from their GP (Teljeur et al., 2010) and are known to make less use of medical services, in RoI at least (Morrissey et al., 2008) and this may account for some of the difference. In Ireland as a whole, there was a clear correlation between higher NMSC risk and area measures of affluence such as higher educational attainment (both sexes) and higher employment (men). This relationship may be due to a greater use of medical services (both primary and secondary care in more educated and/or more prosperous populations. People with lower incomes are significantly less likely to be referred to a specialist (van Doorslaer et al., 2006; McBride et al., 2010).
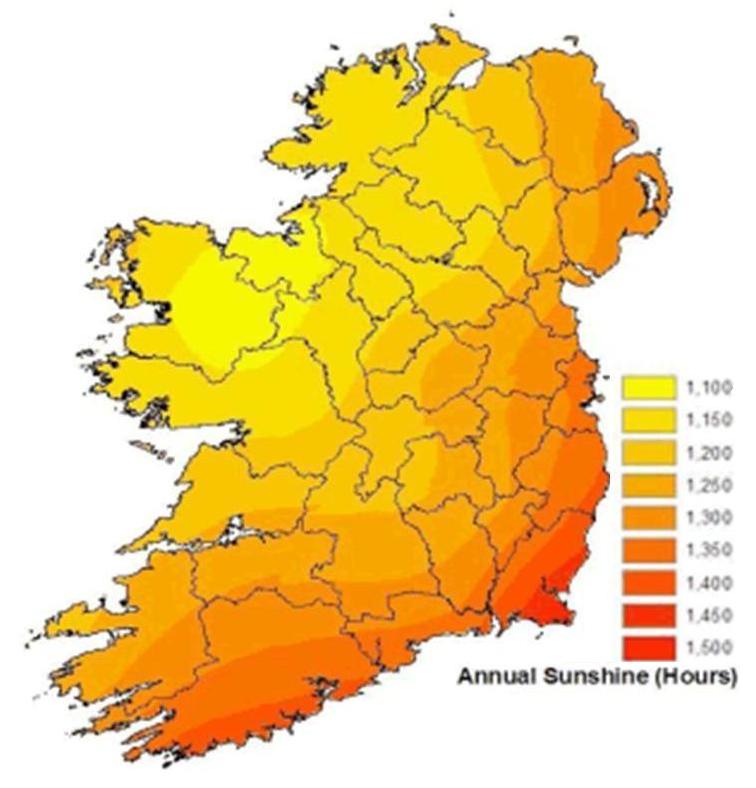
The coastal pattern has no obvious explanation. Some of the areas of higher risk coincide with the location of fishing ports (Map 21.1) (Department of Agriculture and Rural Development, 2011; Department of Agriculture, Fisheries and Food, 2011) but the low numbers employed in fishing and the similarity of patterns between men and women make fishing an unlikely explanation. Migration of retired people to seaside areas also seems unlikely to have occurred at a rate which would explain the large differences in risk observed. Relatively few areas of high NMSC risk exist in areas of low sunshine (Map 21.2); however the relationship between higher sunshine levels and NMSC risk is not consistent. Areas in the south-east with high sunshine levels (by Irish standards) have low NMSC risk (Map 21.2). The higher risk in north and west Kerry and in Newry and Mourne is difficult to explain solely in terms of annual sunshine. Other factors related to coastal location may play a part. Areas around the coast may be less shaded from the sun and may also have features such as coastal walks, mountains etc. that draw residents out of their homes more, and for longer periods.
| Map 21.1 Relative risk of non-melanoma skin cancer (both sexes) and location of larger fishing ports | |
| relative risk of non-melanoma skin cancer (both sexes) | location of larger fishing ports |
 |  |
| Map 21.2 Relative risk of non-melanoma skin cancer (both sexes ) and annual sunshine 1961-1990 | |
| relative risk of non-melanoma skin cancer (both sexes) | annual sunshine 1961-1990 |
 | 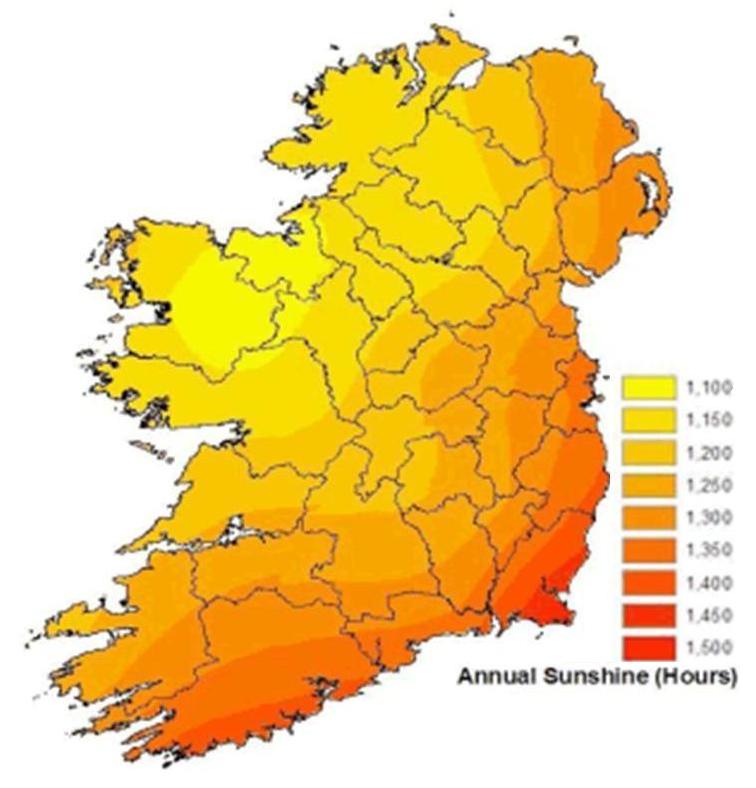 |
Note: Sunshine data from Met Eireann http://www.met.ie/climate-ireland/sunshine.asp [1] | |
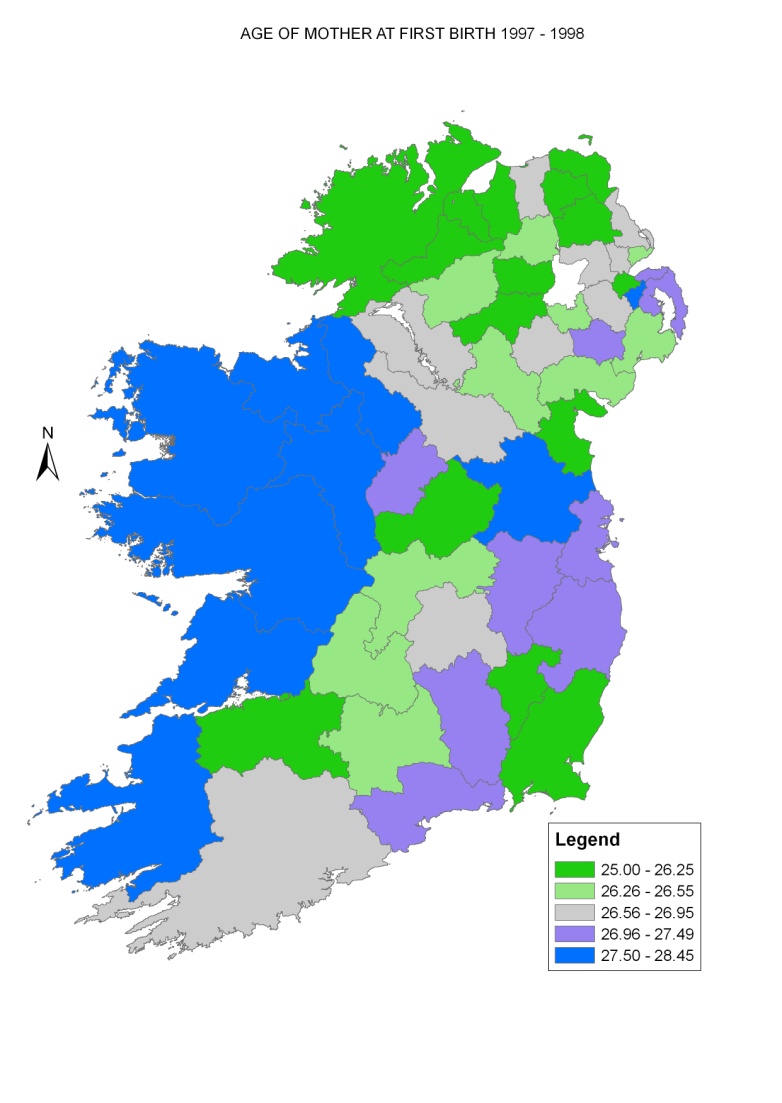
The major aetiological factor for breast cancer is lifetime average oestrogen exposure, from both endogenous and exogenous sources (Veronesi et al., 2005 Key et al., 2001, International Agency for Research on Cancer, 2011a). Protection is afforded by breastfeeding and full-term pregnancies at an early age. Increased risk has been shown to be positively related to affluence. This relationship is likely to be due to a number of reasons, including patterns of childbearing, post-menopausal use of hormone replacement therapy and obesity. The average age at first birth in RoI fell from 27.5 in 1975 to 24.8 in 1995, but rose thereafter to its 2009 level of 29.1. In the 1990s, age at first birth tended to be higher in the west of RoI and relatively low in NI, with the exception of Castlereagh, North Down and Ards (Map 21.3).
Map 21.3 Average age of mother at first birth, RoI 1989-1998, NI 1997-1998
The relationship between employment levels and breast cancer risk found here was modest; that with educational levels was stronger. However, ascertainment bias due to screening may have had the effect of masking the relatively modest differentials in risk caused by socio-economic factors. The overall variation in risk across Ireland was relatively small.
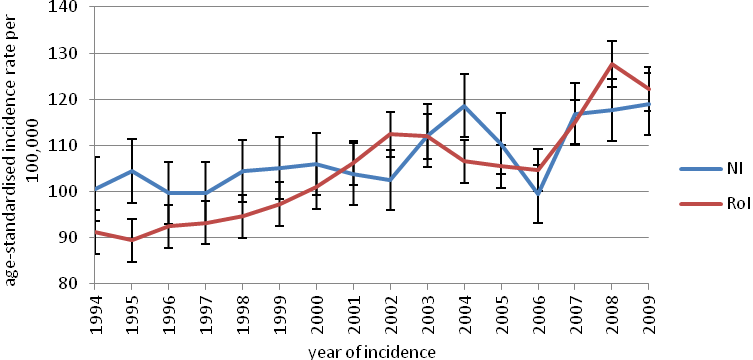
Map 4.2 shows a clear gradient in 1995-2001 between higher risk in NI, where breast screening began in 1989 (HSC Public Health Agency, 2011), and lower risk in RoI, where screening began only in 2000 (National Cancer Screening Service, 2010) and then only in the eastern half of the country. Observed incidence rates were higher in NI up to 2000, but became higher in RoI from 2001 on (National Cancer Registry, 2011, Donnelly et al, 2010) (Figure 21.3). The introduction of population-based breast screening is the most likely explanation for the increase in incidence in RoI (Møller et al., 2005).
In both countries, socio-economic and geographical differences in incidence may also result from variations in screening coverage and compliance. Given the long history of breast screening in NI, the higher risk seen north and east of Derry, to the east of Belfast and in Newry and Mourne is likely to reflect a true difference in risk rather than an artefact due to screening. In RoI, in the period before organised screening began, the risk was higher in urban areas and, in Dublin, in the more affluent areas to the east and south of the city. Once population-based screening was established in RoI the areas of higher risk became more extensive. The area of higher risk in south Dublin seen during 1995-2001 was much less defined in 2002-2007, and extended to cover most of Dublin, Kildare, Louth and Meath. An area of above-average risk can also be seen in a triangle bounded by Cork, Waterford and Athlone. However, many areas in the east which would have been covered by screening in the east did not show as great an increase in relative risk.
Figure 21.3 Trends in female breast cancer incidence for RoI and NI 1994-2009 (European age-standardised incidence rates ± 95% confidence limits)
The aetiology of colorectal cancer is multifactorial, with lifestyle having a major role; smoking (colon cancer only) (Secretan et al., 2009), alcohol (Secretan et al., 2009), obesity (International Agency for Research on Cancer, 2002), some aspects of diet and physical inactivity (World Cancer Research Fund/American Institute for Cancer Research, 2007) have been shown to be risk factors, while use of hormone replacement therapy and oral contraceptives (International Agency for Research on Cancer, 2011a) and non-steroidal anti-inflammatory drugs (International Agency for Research on Cancer, 1997) have been shown to be protective. RoI had a slightly higher risk for men than NI, when adjusted for factors such as population density and unemployment. The risk was correlated with population density and unemployment for men, but there was only a modest variation in risk across the island. The area of higher risk in Cork and along the south coast was common to men and women. An area of higher risk across most of NI (apart from the area around Belfast) and in Donegal, and of low risk in Connacht, was seen for women only while the areas of higher risk in Dublin, Meath and Louth were seen for men only . As the incidence of colorectal cancer is considerably higher in men than in women, the prevalence of important aetiological factors seems to be different for the two sexes, or at least to affect risk in different ways. One difference suggested has been the protective effect of hormone replacement therapy and oral contraceptives (dos Santos Silva and Swerdlow, 1996). We do not have enough information on the geographical variation of these factors between the sexes to be able to interpret the geographical patterns shown; however the higher overall female risk in rural NI and around Cork is worthy of further investigation.
Smoking is the single most important risk factor for lung cancer (International Agency for Research on Cancer, 2004b), and the distribution of the cancer is likely to closely mimic that of smoking prevalence 15-20 years before the period reported here; that is, between 1975 and 1987. However, there is little available information on smoking prevalence for that period. Lung cancer risk was slightly higher in NI and showed the expected correlation with higher population density, higher unemployment and lower educational attainment. In NI the geographical pattern of lung cancer was similar for both sexes, and the higher risk was largely confined to Belfast, Derry and Newry. In RoI there were four areas of higher risk outside the main urban areas—in south Kildare and south Wicklow, around Mullingar in Westmeath and in south-east Limerick. The areas of higher risk for women were more concentrated along the east coast than those for men.
Radon levels may explain some of the geographical variation in risk, but as noted in a previous report (Carsin et al., 2009), there was no apparent correlation between areas of high lung cancer risk in RoI and average household radon levels. A lack of relationship between lung cancer risk and area measures of radon exposure has been a consistent finding of ecological studies (Puskin, 2003), partly because of the strong confounding effect of smoking (which is responsible for over 90% of lung cancers) and partly because individual exposures to radon are poorly correlated to area averages.
Relatively little is known of the role of lifestyle and other potentially modifiable factors in prostate cancer aetiology, despite intensive investigation. The use of prostate-specific antigen (PSA) testing on a widespread scale in asymptomatic men has uncovered large numbers of occult carcinomas and has led to increases in incidence rates all over the developed world (Quinn and Babb, 2002). In Ireland, the prostate cancer incidence rate increased markedly over the study period. The consequence has been to mask any differences in underlying risk. The risk of prostate cancer was considerably higher in RoI than in NI and, unlike almost every other cancer, the risk had an inverse relationship with population density. The risk of prostate cancer was also higher in areas with higher education levels.
Mapping of prostate cancer risk in 1995-2001 showed a relatively lower rate of risk in NI compared to RoI and, in RoI, a patchy distribution with no overall pattern. While the rate was high in and around some urban areas, in others (e.g. Limerick) there was no evidence of increased risk. In Dublin, there was a markedly higher risk in the south, and especially the south-west, of the city. This distribution had a closer resemblance to patterns of educational attainment than to unemployment (see Maps 2.4 and 2.5). In 2002-2007 the spatial pattern in RoI showed, to a large extent, an extension of the areas of higher risk to the more rural parts of the country and a lessening of the north-south differential in Dublin city. In NI, some areas of higher risk in the west had disappeared in the later period, but this may be an artefact due to the fact that risk in other areas had increased in 2002-2007.
Although the GP referral guidelines from the National Cancer Control Programme (RoI) (Health Service Executive, 2011) state that “PSA testing of asymptomatic men or PSA screening is not national policy” this seems to have had only a limited impact on practice in RoI, where PSA testing was at a very high level during the period covered by the atlas (Drummond et al., 2010). The differences in overall prostate cancer risk between RoI and NI seem to be determined by higher rates of PSA testing and a lower threshold for prostate biopsy in RoI (Carsin et al., 2010). The changes in geographical patterns of risk within RoI are likely to reflect changes in testing and biopsy rates, due to a combination of awareness and implementation of policy by GPs, demands by patients and investigation rates by specialists. Of interest is the noticeable fall in relative risk between 1995-2001 and 2002-2007 in the former RoI South Eastern Health Board area (counties Waterford, Kilkenny, Wexford, Carlow and Tipperary South). It would be interesting to investigate which, if any of the factors listed above were responsible for this change.
Non-Hodgkin’s lymphoma consists of a number of malignancies of the lymphatic system with differing patterns of incidence by age and sex, differing clinical courses and probably differing aetiologies. Both men and women in NI had a higher risk, but this was statistically significant only for women. There was little variation in risk by any of the socio-demographic variables studied. Geographical variation in risk was modest. The overall geographical pattern was the same for men and women, although more obvious for women, with an area of highest risk in eastern NI, extending through Louth and Meath to north Co. Dublin.
Stomach cancer risk, which is linked to diet (World Cancer Research Fund/American Institute for Cancer Research, 2007), smoking (Secretan et al., 2009) and H pylori infection (International Agency for Research on Cancer, 1994) was strongly correlated with higher population density, higher levels of unemployment and lower levels of educational attainment, for both men and women. Crowded housing appears to be related to higher rates of H pylori infection (Brown, 2000), consistent with the observed association with population density. There was no significant difference in risk between NI and RoI. Overall geographical variation was marked, and similar for men and women. For women a band of higher risk was seen from north Dublin, through Louth, Cavan, Monaghan and west Fermanagh to Donegal. This increased risk was almost entirely on the RoI side of the border. For men, there was no area of increased risk in Fermanagh, and the high relative risk was almost entirely confined to RoI. For both men and women there was an area of higher risk in Belfast city (which presumably explains the similar risk in RoI and NI despite the pattern described above) and for women a few isolated areas of higher risk in west Kerry, west Galway and Wicklow.
As H pylori is easily diagnosed and treated, the relationship between H pylori prevalence rates and geographical variation in stomach cancer should be investigated at a community level.
As with non-melanoma skin cancer (NMSC), UV exposure causes melanoma of the skin (International Agency for Research on Cancer, 2001; Armstrong and Kricker, 2001). However, screening or case-finding may increase the number of early lesions detected and may confound the effects of sun exposure to some extent. As it is generally accepted that NMSC risk depends largely on lifetime exposure to UV radiation, while melanoma is related to recreational and intermittent exposure (International Agency for Research on Cancer, 2001; Armstrong and Kricker, 2001), it would be expected that their distribution patterns would differ somewhat.
| Map 21.4 Relative risk of melanoma 1994-2007 and annual sunshine hours 1961-1990 | |
| Relative risk of melanoma (both sexes ) | Average hours of sunshine 1961-1990 |
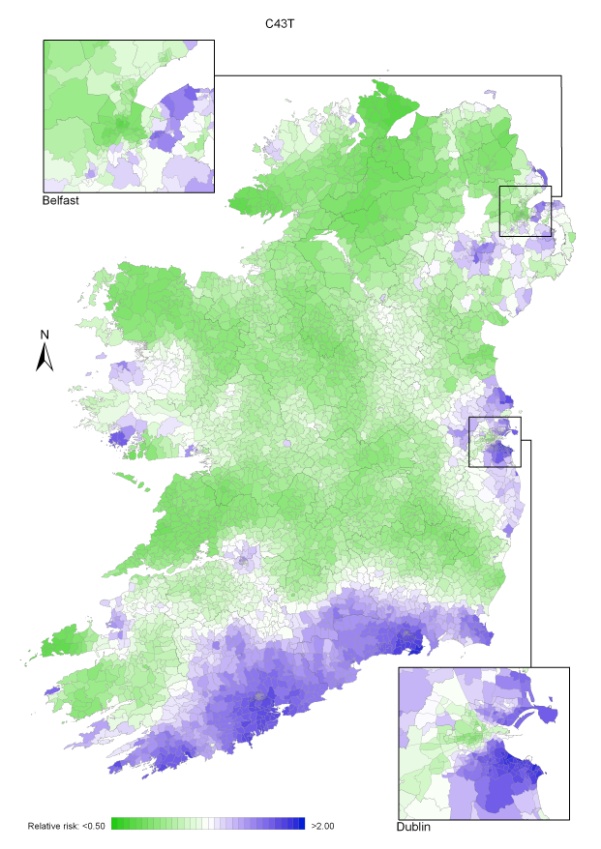 |  |
| Source: Sunshine data from Met Eireann http://www.met.ie/climate-ireland/sunshine.asp [1] | |
As with NMSC, there was a higher risk in RoI than in NI; melanoma had a weaker relationship to population density and a stronger relationship to measures of affluence, than did NMSC. Because the number of cases was much lower for melanoma, small geographical variations in risk have been smoothed to a greater extent than for NMSC. Nevertheless, both similarities and differences can be seen. There was an area of high melanoma risk to the east of Belfast for both men and women which was not seen for NMSC, with a second area of higher risk around Craigavon. In NI, these areas are close to hospitals and may reflect case finding.
In RoI there was a clear band of higher risk running from south Wexford through Waterford to west Cork for both men and women, but the areas of higher risk observed for NMSC along the western seaboard were much less in evidence, especially for men. The pattern of risk in Dublin was similar to that for NMSC, with higher risk to the north and south of the city centre.
Despite the possible role of detection, ascertainment bias is unlikely to have played a major role in the geographical variations seen here and, as with NMSC, it is difficult to interpret the patterns either in terms of susceptibility, or of natural UV exposure at the place of residence. The socio-economic variation, and geographical variation in Belfast and Dublin, is almost certainly due to difference in holidaying practice two decades ago (Corcoran et al., 1996), but the higher risk along the south coast is more difficult to explain. However, there appears to be a stronger relationship with average sunshine levels than was seen for non-melanoma skin cancer (Map 21.4). A similar north-south gradient in melanoma risk has been reported in England (Quinn et al., 2005).
The risk of bladder cancer in RoI was higher than in NI. The risk of bladder cancer increased with population density but had only a weak relationship to unemployment or education levels for either men or women. For women, there were areas of higher risk in and around the major urban areas of Belfast, Dublin, Cork and Limerick, but not Derry or Galway. The area of higher risk around Limerick was unusual, as Limerick was not consistently among the urban areas with higher risk for other cancers. There was no clear geographical distribution in Dublin, but in Belfast the highest risk was in the east and central part of the city. An almost identical urban pattern was seen for men.
Outside the cities, both men and women had a higher risk on the east coast from Dublin to Wicklow, particularly for men, and in north and west Kerry, particularly for women. There was a high male risk in Donegal and the Ards peninsula, much less so for women.
Bladder cancer risk has been strongly linked to tobacco smoking (Secretan et al., 2009) and there was a limited degree of similarity between the distribution of lung cancer and bladder cancer. Occupational exposure is also an important risk factor (Baan et al., 2009). While most exposures are now controlled, historical exposure to occupational carcinogens (for instance in the chemical, rubber, dyeing and tanning industries) may be responsible for some of the variation seen; there is little information on historical exposures in Ireland.
Head and neck cancer is a heterogeneous group of cancers, but with a largely shared aetiology in tobacco and alcohol use (Secretan et al., 2009). In recent years, human papilloma virus infection is likely to have been responsible for an increasing number of cases, particularly cancers of the tonsil (International Agency for Research on Cancer, 2011b).
The risk of head and neck cancer was higher in NI for women but not men. For both sexes there was a strong relationship to unemployment levels, but not to education. For women there was a band of higher risk extending from north Dublin through Louth into Fermanagh. The areas of highest risk, however, were around Belfast, Derry and on the Inishowen and Dingle peninsulas.
For men, the geographic pattern was very different to that observed for women. There was a patchy distribution of higher risk areas, including most major cities and adjoining areas and a number of sparsely populated areas along the west coast. The pattern of risk more closely resembled that of bladder cancer than lung cancer.
The patterns seen most likely reflect a complex interaction between smoking and alcohol use. The consumption of home-distilled alcohol (poitín) in the past may also have been a factor in rural areas. Dentists have a role in detection of pre-malignant lesions and early oral cancers; residents of more deprived areas (Lang et al., 2008) and those with primary education only (Woods et al., 2009) use dentists less and this may be a factor in areas of higher risk.
There was a markedly higher risk of leukaemia in RoI than in NI, a surprising finding given the low level of international variation in Europe and the paucity of modifiable risk factors, other than smoking (Secretan et al., 2009). Some ascertainment bias may exist with respect to chronic lymphocytic leukaemia (CLL), which comprises over 40% of all leukaemias, affects older patients and may be asymptomatic for much of its course. It is often detected only through routine blood counts and only picked up if the individual presents to clinical services. However, it is not clear how these factors would differ between NI and RoI. We could find no information on either GP consultation rates or routine blood count rates for older persons in NI and RoI. Socio-demographic variables were poorly correlated with leukaemia risk; the risk was higher especially for men and women in areas with a higher proportion of older persons living alone. The significance of this finding is obscure.
For both men and women the geographical pattern was of a smooth gradient in risk; lowest in the north-east and highest in the south-west. For men in particular the area of highest risk seemed to centre on Limerick and Clare rather than the extreme south-west and for both sexes there was a secondary area of higher risk extending from south Dublin to Wexford, with the highest risk around Wicklow town.
The north-east to south-west gradient could possibly be due to differences in health service utilization between NI and RoI which impacted on detection of asymptomatic CLL. However, when such a difference between countries was simulated in the smoothing process it gave rise to a much sharper gradient in risk at the border than was seen in the leukaemia maps.
The risk for pancreatic cancer, which is associated with tobacco and heavy alcohol use (Secretan et al. 2009), was significantly higher in RoI than in NI for men and women. Pancreatic cancer is rapidly fatal and the diagnosis is not always confirmed before death, so there is more uncertainty with regard to the reliability of diagnosis than for most other cancers. However, mortality rates in 1995-2007 were also higher for both men and women in RoI than in NI (International Agency for Research on Cancer, 2011c).
For men, the risk fell (but not significantly) with increasing population density but increased with increasing unemployment. For women, on the other hand, the risk was unrelated to population density or unemployment but was higher in areas with a lower level of educational attainment.
The overall geographical pattern was, however, similar for men and women—a smooth gradient from the lowest levels in the north-east to the highest in the south-west, centred, for women, in north Kerry and, for men, on Cork city. For women, there appeared to be a higher risk in central and north Dublin city, but a uniformly low risk in Belfast. For men, the risk in Dublin city was low relative to the rest of the country; although the risk was also low in Belfast, the city centre had a slightly higher rate than the outskirts.
The important aetiological factors for kidney cancer are smoking (Secretan et al., 2009) and obesity (World Cancer Research Fund/American Institute for Cancer Research, 2007). The risk of kidney cancer was slightly (but not significantly) lower in NI than in RoI for men, but not women. There was a weak upward trend in risk with population density for women but no other relationship to socio-demographic variables.
While for both sexes there was an area of higher risk along the east coast—in Wicklow, Dublin, Meath and Louth—the overall pattern of risk was different for men and women. For women, there was an extensive area of higher risk in northern NI, while for men the risk in NI was lower, apart from Fermanagh. For men there was an extensive area of higher risk in the east midlands, extending into Galway, with the highest risk in Offaly. There was no clear intra-urban pattern for either sex.
Increasing numbers of kidney cancers are being detected incidentally in the course of abdominal scans for other disease (Hock et al., 2002; Falebita et al., 2009) and this may affect geographical patterns.
Cancer of the oesophagus consists of two main histological types—squamous carcinoma and adenocarcinoma—which differ somewhat in their underlying causes. While both are related to tobacco and alcohol consumption (Secretan et al., 2009), only adenocarcinoma is related to obesity (World Cancer Research Fund/American Institute for Cancer Research, 2007). As the analyses in this atlas combine these cancer types, this might have obscured some patterns specific to one or other histological type.
For both men and women there was an increase in risk with increasing population density and for men, a weak relationship to unemployment.
The pattern of distribution of oesophageal cancer was similar for men and women. The highest risk in the urban areas was in Dublin and Belfast city centres, although the female risk was lower in Belfast than Dublin. There was no area of high risk associated with other urban centres, other than the region around Cork.
Outside Dublin and Belfast, there seemed to be three main foci of higher risk—the largest around Cork city, extending, for women, to the east and west and, for men, to the north, into Tipperary. The second focus was in south Dublin and Kildare and was more defined for men than for women. The third area was smaller, involving Larne, Belfast, Ards and (for men) north Down. There were also two small areas of higher risk for men around Drogheda and Dun Laoghaire.
Family history is the most important risk factor for ovarian cancer (Stratton et al., 1998); potentially modifiable risk factors include nulliparity, age at first pregnancy and number of pregnancies (Ness et al., 2002; Nagle et al., 2008; Jordan et al., 2007). Obesity may also be a risk factor (Schouten et al., 2008). The risk was similar in RoI and NI, and none of the socio-demographic variables studied appeared to correlate with risk.
The incidence of ovarian cancer is particularly high in Ireland and the UK compared with many other developed countries. However, differentiation between frankly malignant and “borderline” ovarian cancer (which is not registered by some cancer registries) is sometimes difficult to make; the resulting variations in registration may contribute to differences in recorded rates internationally.
Two areas of higher risk were found; one to the east of Cork city extending through most of Cork and Waterford, and the other a more diffuse area in NI encompassing Moyle, Ballymoney and Ballymena, Dungannon/Craigavon, Down and part of Newry and Mourne. The relative risk was low in the Belfast area.
The pattern of risk bears some resemblance to that of colorectal cancer, which also was poorly correlated with socio-economic variables, as well as to oesophageal cancer; the latter, however, was also related to population density and unemployment.
The aetiology of brain and other central nervous system cancers is largely unknown. There is very little international variation apart from the high incidence in the Nordic countries, and, within Ireland, there was only a minor degree of geographical variation. For both men and women there was a gradient of risk, lowest in the north-east and highest in the extreme south-west, reflected in an overall higher risk in RoI. The extent of variation was greater for women than men but otherwise the patterns were almost identical.
Modifiable risk factors for cancer of corpus uteri include obesity (World Cancer Research Fund/American Institute for Cancer Research, 2007), nulliparity (Dossus et al., 2010) and use of hormone replacement therapy and tamoxifen (International Agency for Research on Cancer, 2011a). The risk of uterine cancer was higher in NI than RoI but showed no significant relationship to any of the socio-demographic variables studied. The geographical pattern was unusual, with two areas of higher risk—one in the eastern part of NI, with the highest rate in Newry and Mourne; the other in the west, with the highest rate in west Mayo, extending into Galway and Sligo. An area of higher risk was also noted in Kerry.
International variations in uterine cancer incidence reflect, to some extent, variations in the prevalence of hysterectomy (Bray et al., 2005). However, we are not aware of any data on the frequency of hysterectomy in NI compared to RoI, or within either country.
The risk of cervical cancer was higher in RoI than in NI, and the incidence rate was relatively high by international standards. The risk was strongly correlated at an area level with increasing population density, unemployment and low educational achievement. A population-based screening programme has been in existence in NI for many years, with all eligible women invited regularly since 1993. In RoI, by contrast, national population-based screening did not begin until 2008, although considerable opportunistic screening has been done for some time.
The highest risk in Belfast was in the north and west of the city, as well as in the city centre, while in Dublin the city centre had the lowest risk. Outside the two major cities there was a large area of higher risk in Kildare, Wicklow and Wexford, an area of higher risk to the north and east of Belfast, and a more diffuse area between Cork and Waterford cities. This distribution was broadly similar to that of lung cancer in women, reflecting their common association with both deprivation and smoking. Prior to the introduction of population-based screening in RoI, the uptake of screening was higher in areas with higher socio-economic status (Walsh et al., 2011); this dependence on socio-economic status appears to be a characteristic of opportunistic screening, as compared to population-based programmes (Walsh et al., 2010).