Current Size: 100%
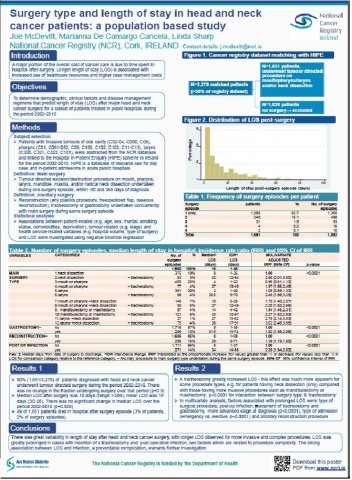
Surgery type and length of stay in head and neck cancer patients: a population based study
Background: In-patient hospital care constitutes the majority of the cost of cancer treatment borne by the health services. Surgical excision, where appropriate, is the main treatment modality in the management of head and neck cancer (HNC). We investigated predictors of post-surgical hospital length-of-stay (LOS) in HNC.
Methods: From NCRI and hospital in-patient enquiry (HIPE) records, we identified patients diagnosed 2002-2010 with primary tumours of the oral cavity (ICD03, C02-04, C050, C06), pharynx (C01, C051-052, C09, C100,C102, C103, C11-C13) or larynx (C32, C101) who underwent tumour-directed surgery with or without neck dissection (ICD9-CM, 24, 25, 27-30, 40, 76) in a public hospital. LOS was calculated as days elapsed between dates of procedure and discharge. Associations between patient-related (e.g. age, marital, smoking status, comorbidities, deprivation, health insurance status), tumour-related (e.g. stage, grade) and health service-related (e.g. hospital volume, type of surgery, radiotherapy) variables and LOS were investigated using negative binomial regression with adjustment for clustering.
Results: Half (1,651/3,279) of HNC patients had tumour-directed surgery. 17% of these underwent more than one surgical procedure. Procedures were classified as: neck dissection only (22%), mouth/pharyngectomy (27%), laryngectomy (24%), mouth/pharyngectomy+neck dissection (12%), mandibulectomy/maxillectomy (10%), laryngectomy+neck dissection (5%). Median LOS was 10 days (range: 1-289, mean: 19). In multivariate analysis, the strongest predictors of longer LOS were:
(1) Undergoing a procedure requiring a tracheostomy, e.g., neck dissection only: median LOS= 8 days; neck dissection+laryngectomy+tracheostomy: median LOS=38 days, incident rate ratio (IRR) 3.0 (95%CI: 2.5-3.7). (2) Post-operative infection, i.e., no infection: median LOS=8 days; infection: median LOS=34 days, IRR=2.3, 95%CI 2.0-2.6). Other significant predictors of longer LOS were ancillary gastrostomy, advanced stage, emergency admission.
Conclusions: Median LOS was longer than for some other cancers probably, in part, reflecting the complex nature of the surgery and the patients’ health status. Indeed, the significant predictors of longer LOS largely reflect procedure complexity. The strong association between LOS and infection, a preventable complication, warrants further investigation.